Characterizing localized retinal layer changes in AMD
Investigators tested the hypothesis that changes in certain areas of the macular are more relevant to AMD. What did their findings reveal?
This article was reviewed by Mengyu Wang, PhD.
The impact of age-related macular degeneration (AMD) on macular retinal layer thickness is highly location-specific, according to results of a population-based study reported by Mengyu Wang, PhD, along with his collaborators Tobias Elze, PhD and Franziska G. Rauscher, PhD, at ARVO 2020.
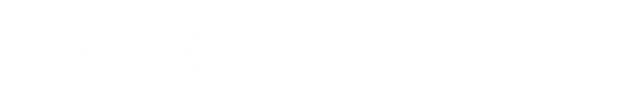
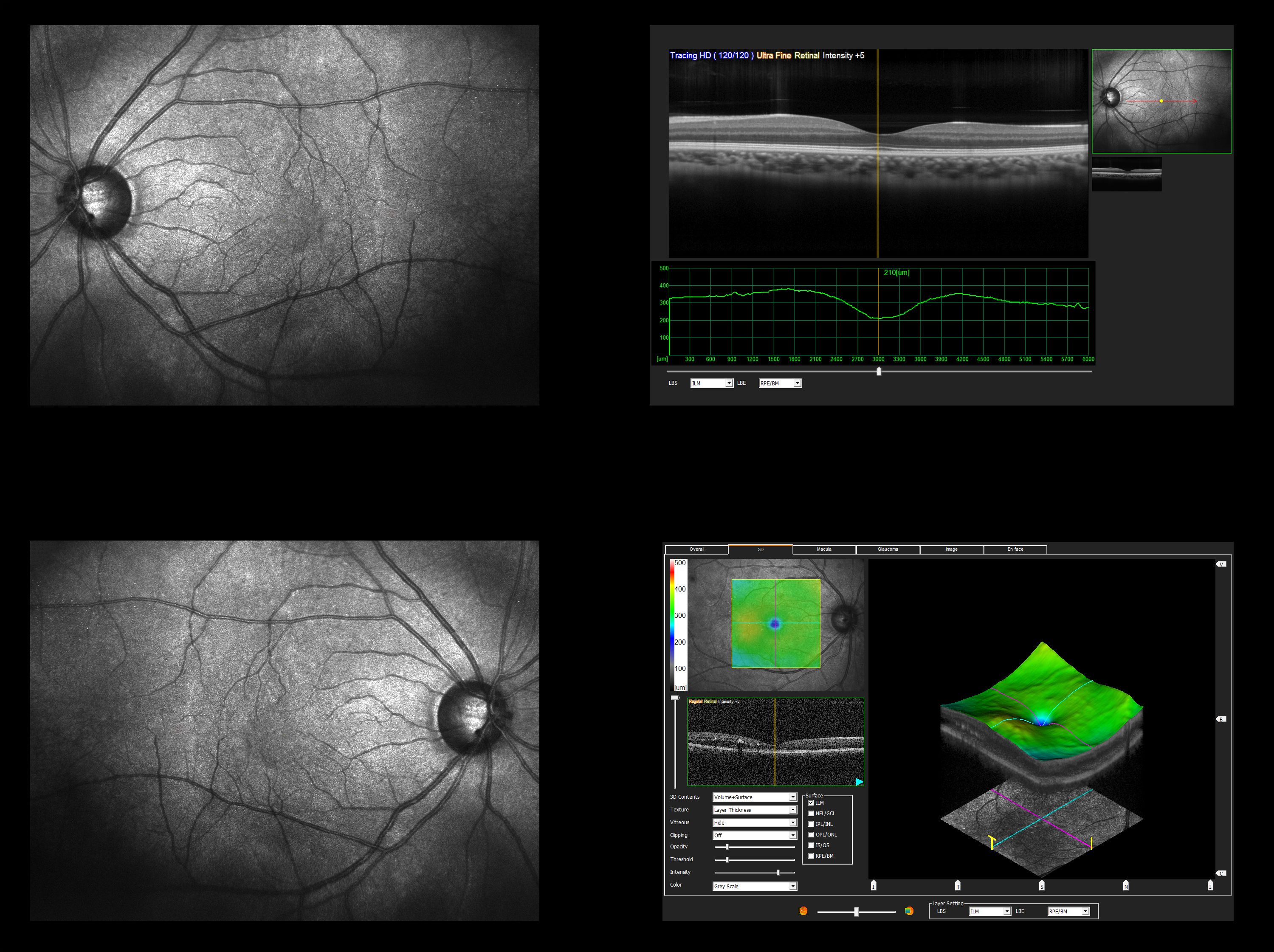
Aiming to test the hypothesis that changes in certain areas of the macular are more relevant to AMD, Wang and co-workers analyzed retinal layer thickness maps (RLTMs) and calculated pointwise partial correlations between the RLTMs and AMD stage. The OCT scans were machine-segmented into 10 layers, including retinal nerve fiber layer (RNFL), ganglion cell layer (GCL), inner plexiform layer (IPL), inner nuclear layer (INL), outer plexiform layer (OPL), outer nuclear layer (ONL), myoid zone (MZ) of the photoreceptors, ellipsoid zone (EZ) of the photoreceptors, and outer segment (OS) the photoreceptors and retinal pigment epithelium (RPE).
In general, the results showed thinning of the ONL, GCL, and IPL in eyes with late dry and wet AMD. The thinning effect showed a parafoveal pattern, and the associations were more substantial for late dry AMD versus wet AMD.
Early and intermediate AMD were largely associated with thicker GCL, outer plexiform layer (OPL), and IPL changes. Considerable areas of the retinal pigment epithelium (RPE) layer were significantly thicker in eyes with late dry and wet AMD, whereas no RPE regions were significantly correlated to early or intermediate AMD, said Wang, instructor in ophthalmology, Schepens Eye Research Institute, Massachusetts Eye and Ear and Harvard Medical School, Boston.
“Traditionally AMD is diagnosed and staged based on fundus inspection of the macula. However, the pathological changes of AMD occur deeper in the retina. Three-dimensional (3-D) imaging with OCT has been widely researched for opportunities to study the relationships between 3-D retinal structure and AMD, and various publications describe associations between the average thickness of retinal layers in the macula and AMD or its progression. However, because the retinal layer damage is typically localized, global averaging is not optimal,” Wang said, explaining the background for the study.
“Therefore, we take advantage of the enriched information of retinal structure in OCT measurements by taking the spatial variation of layer thickness into consideration. In the long run, we aim to develop AMD diagnostic methods based on OCT volume scans as opposed to current clinical approaches focused on fundus images. Three dimensional ‘in-depth’ retinal imaging contains considerably more ophthalmic information than 2-D fundus imaging, and the importance of many of these additional details for understanding, diagnosing, and monitoring AMD is still unclear. Our study sheds light on these aspects,” Rauscher said.
All data used in the study are from the Leipzig Research Centre for Civilization Diseases—LIFE Adult study. The Principle Investigator of the LIFE Adult study is Professor Markus Loeffler, Institute for Medical Informatics, Statistics and Epidemiology, Leipzig University, Leipzig, Germany. The eye examination of this population-based study is led by Dr. Rauscher of the same institute.
The study was conducted using spectral-domain OCT (Spectralis, Heidelberg) scans of the macula from 1625 eyes of 1625 subjects who were participants in the LIFE-Adult population-based study conducted by Leipzig University. In choosing which eye from each participant to include in the study, preference was given to the worst eye. AMD stage was graded by trained graders who evaluated the OCT fundus image supplemented by further examination of corresponding OCT B-scans. Using the Rotterdam classification, the cohort included 537 non-AMD eyes, 668 eyes with early (drusen size < 125 μm) or intermediate (drusen size ≥ 125 μm), 55 eyes with late dry AMD and 365 eyes with wet AMD.
The analyses of pointwise partial correlations between the RLTMs and AMD stage were adjusted for age, gender, and glaucoma diagnosis.
“In our study, age was generally negatively correlated with layer thickness with the exception of the OS layer. Male gender was generally related to a thinner RNFL and thicker ellipsoid zone, while glaucoma was mostly related to a thinner ONL and thicker RPE,” Wang said.
The results for the analyses of correlations between AMD stage and RLTMs showed that early/intermediate AMD was most substantially associated with GCL, OPL, and IPL, significantly affecting 24%, 13%, and 8% of the scanned region with extensive positive associations. Late dry AMD was most substantially associated with the ONL, GCL, and IPL with largely negative correlations affecting 60%, 34%, and 12 % of the scan region. In addition, late dry AMD showed an extensive positive correlation with the RPE, affecting 24% of the scan region. Wet AMD was associated with RPE layer changes with a largely positive correlation affecting 81% of the scan region. Wet AMD was also associated with ONL changes affecting 21% of the scan region that were mainly negative in the parafovea. The GCL and IPL also correlated with wet AMD in the parafovea, but without statistical significance after adjustment for multiple comparisons.