Authors: Robert P. Finger1, Taiji Sakamoto2, James Talks3, Vincent Daien4,5, Tien Wong6,7, Bora Eldem8, Paul Mitchell9, Jean-François Korobelnik10,11
1 - Department of Ophthalmology, University of Bonn, Bonn, Germany
2 - Department of Ophthalmology, Kagoshima University Graduate School of Medical and Dental Sciences, Kagoshima, and J-CREST, Japan
3 - Department of Ophthalmology, Royal Victoria Infirmary, Newcastle upon Tyne, United Kingdom
4 - Department of Ophthalmology, Gui De Chauliac Hospital, Montpellier, France
5 - The Save Sight Institute, Sydney Medical School, The University of Sydney, Sydney, NSW, Australia
6 - Singapore Eye Research Institute, Singapore National Eye Centre, Singapore, Singapore
7 - Duke-NUS Medical School, Singapore, Singapore
8 - Faculty of Medicine, Ophthalmology Department, Hacettepe University, Ankara, Turkey
9 - Centre for Vision Research, Westmead Institute for Medical Research, University of Sydney, NSW, Australia
10 - CHU Bordeaux, Service d'ophtalmologie, Bordeaux, France
11 - Univ. Bordeaux, Inserm, Bordeaux Population Health Research Center, team LEHA, UMR 1219, F-33000 Bordeaux, France
Disclosures:
R. P. Finger – Consulting/paid presentations for Bayer, Novartis, Roche/Genentech, Novelion, Opthea, Inositec, Santhera, Alimera and Ellex; Research for Novartis, Zeiss and CentreVue; T. Sakamoto – Alcon, Bayer, Novartis, Santen, Senju and Wakamoto; J. S. Talks – Advisory boards for Bayer, Novartis, Allergan; Research for Bayer, Novartis, Allergan and Roche; Travel sponsorships for Bayer and Novartis; V. Daien – Alcon, Bayer, Horus, Novartis and Thea; T. Y. Wong – Abbott, Allergan, Bayer, Novartis, Pfizer and Roche; B. M. Eldem – Consultant to Bayer, Novartis, Allergan and Investigator to Roche; P. Mitchell – Consultant for Bayer, Novartis, Allergan, Roche, Abbott; J.-F. Korobelnik – Alcon, Allergan, Bayer, Beaver Visitec, Horus, Krys, Kanghong, NanoRetina, Novartis, Roche, Thea and Zeiss
The authors have no commercial interests in relation to the article. Medical writing and editorial support for preparation of the article, under the guidance of the authors, was provided by ApotheCom, which was funded by Bayer Consumer Health.
Real-world evidence (RWE) provides an understanding of patient experiences of their disease and treatment beyond the randomised controlled trial (RCT) setting.1,2 In ophthalmology, RWE can help to improve knowledge of the impact of visual impairment and its treatment, aiding the optimisation and customisation of treatment for each patient.3 Ophthalmologists can generate their own RWE by contributing to a larger data source, such as a patient registry, or by conducting studies and clinical audits within their own practice or local area.
What is a clinical audit?
A clinical audit can be used as a process for monitoring aspects of clinical care to ensure they are being carried out as per recognised standards or ‘best practice’. Clinical audits can be conducted for a variety of reasons and can monitor different outcomes. A clinical audit can be a systematic cycle that involves measuring clinical care against specific standards. The aim is to improve the understanding and quality of clinical care, if necessary, and continuously monitor it to sustain those improvements.4
Types of clinical audit
Why generate your own RWD?
In clinical practice, anti-VEGF treatment regimens often differ from the strict regimens used in RCTs. This makes access to RWE particularly important when assessing clinical outcomes from real-world practice. An audit provides the opportunity for clinical care teams to understand their own practice and their patients’ clinical outcomes. It also encourages teams to work together to address any weaknesses that might be uncovered during the audit. The RWD collected during an audit allows the experience of individual clinics to be benchmarked against data from the wider community.
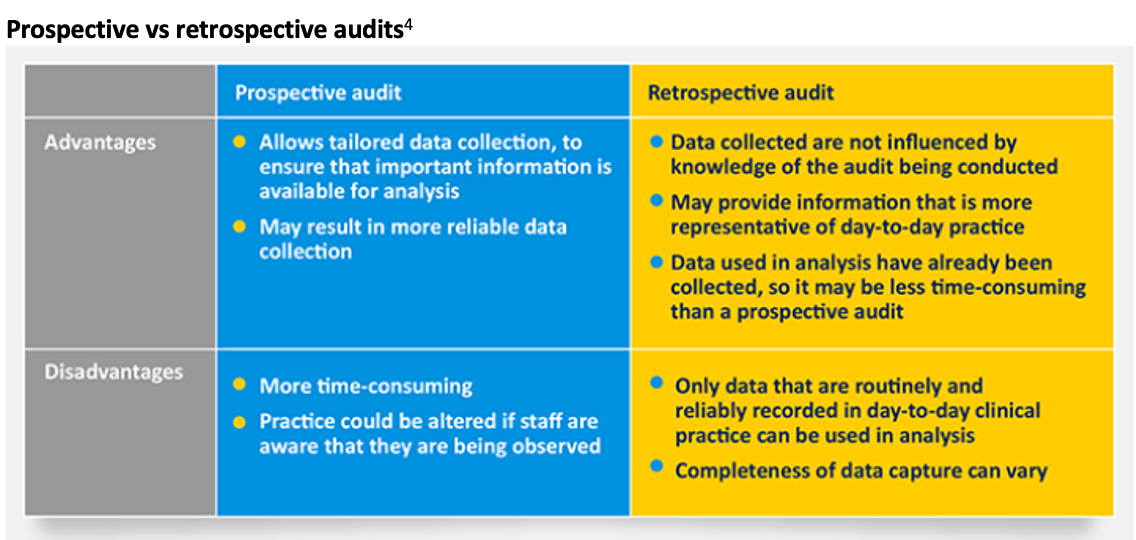
Sharing experience and knowledge about the management of patients with disease phenotypes that are often excluded from RCTs can be particularly helpful. Generation of RWE via a clinical audit helps provide insights into the quality of care locally so that procedures in clinical practice can be optimised. An audit can be either prospective or retrospective, the advantages and disadvantages of which are described in further detail in the table below.4
Key considerations in setting up an audit
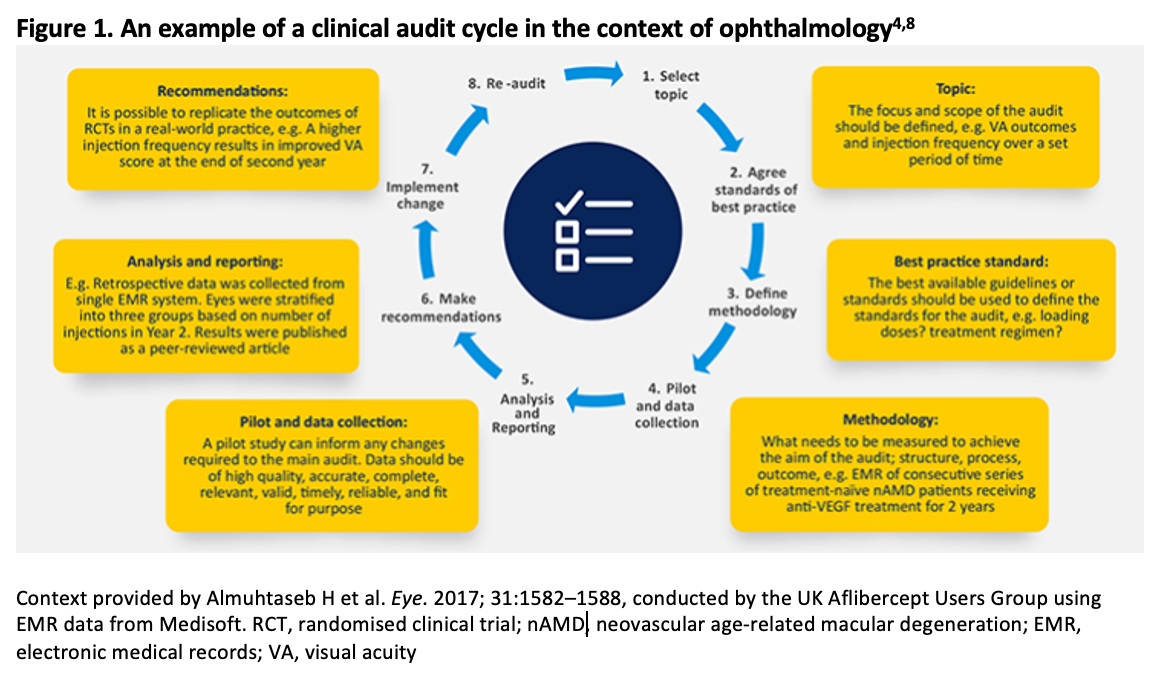
The team conducting an audit should include representatives from all staff involved in the service. The audit can be conducted using data derived from an electronic medical record (EMR) platform, such as the Fight Retinal Blindness! (FRB!) project,5 Medisoft6 or the Intelligent Research in Sight (IRIS®) Registry.7 These platforms allow for information on treatment and clinical outcomes for thousands of patients to be made available, thereby simplifying the process of conducting an audit. Alternatively, where such platforms are not available, audit of reliably captured clinical data can be conducted using patient charts or electronic medical records. The key stages of a clinical audit looking at anti-VEGF use in clinical practice as an example are outlined in Figure 1.
Considerations for setting up an audit in ophthalmology9
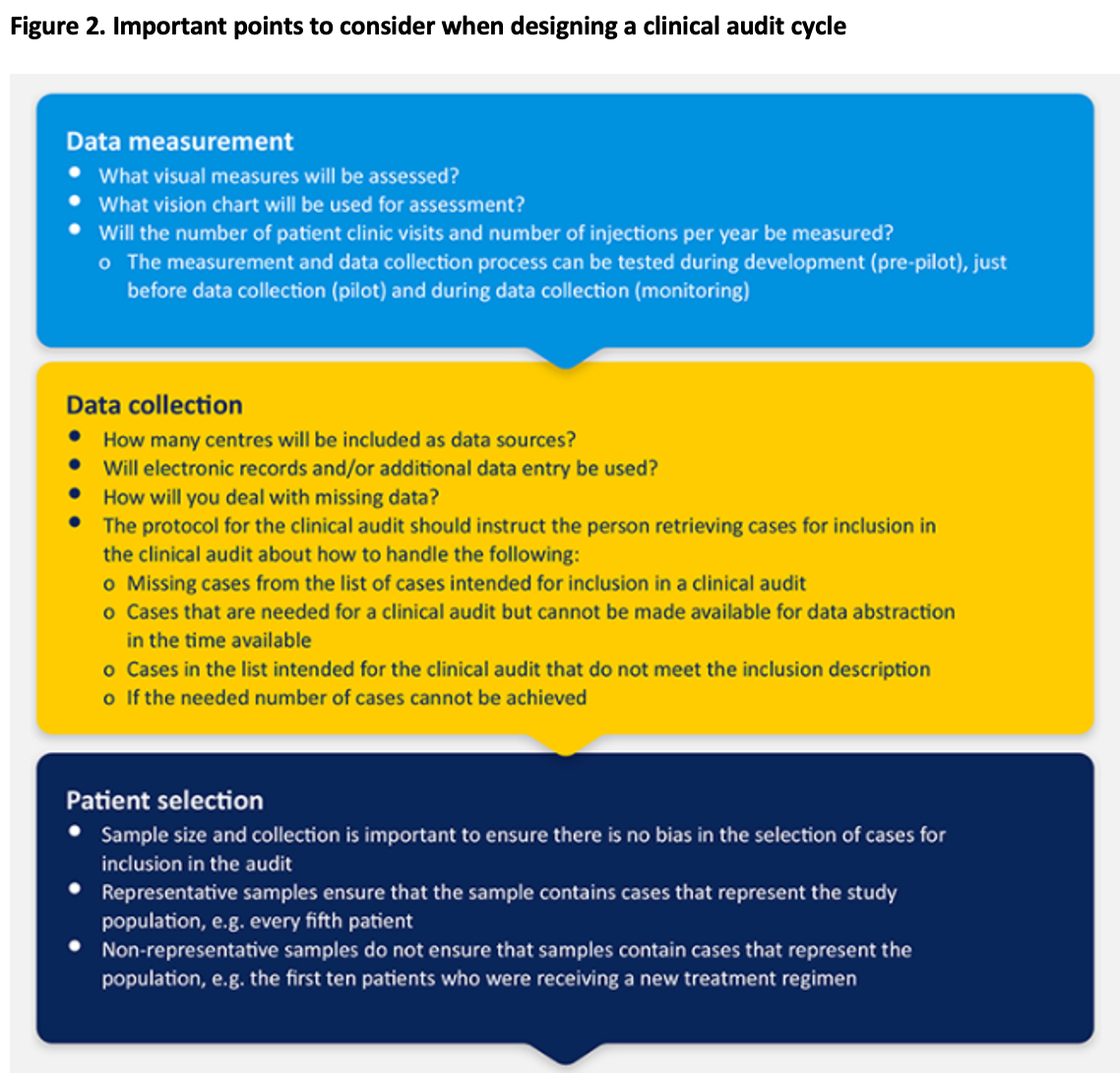
The various aspects specific to clinical audits in ophthalmology that should be considered are highlighted in Figure 2.
Strategies to overcome barriers to multidisciplinary clinical audits
It is important to create the time and space for staff to contribute to data collection and interpretation. Providing training to improve the technical capabilities of staff is key and requires careful planning.
Communication gaps between audit support staff and professional medical staff may arise due to confusion around staff roles within the team, the lack of clearly defined group tasks, and differences in professional backgrounds and priorities.10
Outsourcing of clinical audits is possible if in-house auditing is not feasible. Outsourcing is a convenient option but can have limitations, such as cost and variability in the quality of audit reports generated,11 and time needs to be dedicated to selecting a good auditing team.
Summary
Clinicians can generate useful RWD data at a local and regional level, benchmark against relevant comparators/references and contribute to the growing body of RWE. Taking a proactive role in this process will ensure implementation of clinical guidelines and compliance with the best clinical standards whilst identifying opportunities for enhancing patient care.
References
Garrison LP, Jr., Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value in Health: the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2007;10(5):326-335.
Talks J. Utility of real-world evidence for evaluating anti–vascular endothelial growth factor treatment of neovascular age-related macular degeneration. Survey of Ophthalmology. 2018;In press.
Almuhtaseb H, Johnston RL, Talks JS, Lotery AJ. Second-year visual acuity outcomes of nAMD patients treated with aflibercept: data analysis from the UK Aflibercept Users Group. Eye (Lond). 2017;31(11):1582-1588.
Johnston G, Crombie IK, Davies HT, Alder EM, Millard A. Reviewing audit: barriers and facilitating factors for effective clinical audit. Quality in health care : QHC. 2000;9(1):23-36.
Nixon DR, Flinn NA. Evaluation of contrast sensitivity and other visual function outcomes in neovascular age-related macular degeneration patients after treatment switch to aflibercept from ranibizumab. Clin Ophthalmol. 2017;11:715-721.
Eylea Prescribing information
Name of the medicinal product: Eylea 40 mg/ml solution for injection. (Refer to full SmPC before prescribing.) Composition: Each vial contains 100 µl, equivalent to 4 mg aflibercept. Excipients: Polysorbate 20, Sodium dihydrogen phosphate, monohydrate, Disodium hydrogen phosphate, heptahydrate, Sodium chloride, Sucrose, Water for injection.
Indication: Eylea is indicated for adults for treatment of neovascular (wet) age-related macular degeneration (AMD), visual impairment due to macular oedema secondary to retinal vein occlusion (branch RVO or central RVO), visual impairment due to diabetic macular oedema (DME) and visual impairment due to myopic choroidal neovascularisation (myopic CNV).
Administration and Dosage: For intravitreal injection only. Each vial should only be used for the treatment of a single eye. Extraction of multiple doses from a single vial may increase the risk of contamination and subsequent infection. Administration only by qualified physician experienced in administering intravitreal injections. Recommended dose: 2 mg aflibercept (0.05 ml) equivalent to 50 microlitres. For wet AMD, treatment is initiated with 1 injection per month for 3 consecutive doses. The treatment interval is then extended to 2 months. Based on the physician’s judgement of visual and/or anatomic outcomes, the treatment interval may be maintained at 2 months or further extended using a treat-and-extend dosing regimen, where injection intervals are increased in 2- or 4-weekly increments to maintain stable visual and/or anatomic outcomes. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly to a minimum of 2 months during the first 12 months of treatment. There is no requirement for monitoring between injections. Based on the physician’s judgement the schedule of monitoring visits may be more frequent than the injection visits. Treatment intervals greater than 4 months between injections have not been studied. For RVO (branch RVO or central RVO), after initial injection, treatment is given monthly. The interval between the 2 doses should not be shorter than 1 month. If visual and anatomic outcomes indicate that the patient is not benefiting from continued treatment, Eylea should be discontinued. Monthly treatment continues until maximum visual acuity is achieved and/or there are no signs of disease activity. Three or more consecutive, monthly injections may be needed. Treatment may then be continued with a treat-and-extend regimen with gradually increased treatment intervals to maintain stable visual and/or anatomic outcomes; however, there are insufficient data to conclude on the length of these intervals. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly. The monitoring and treatment schedule should be determined by the treating physician based on the individual patient’s response. Monitoring for disease activity may include clinical examination, functional testing or imaging techniques (e.g. optical coherence tomography or fluorescein angiography). For DME, initiate treatment with 1 injection/month for 5 consecutive doses, followed by 1 injection every 2 months. No requirement for monitoring between injections. After the first 12 months of treatment, and based on visual and/or anatomic outcomes, the treatment interval may be extended such as with a treat-and-extend dosing regimen, where the treatment intervals are gradually increased to maintain stable visual and/or anatomic outcomes; however, there are insufficient data to conclude on the length of these intervals. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly. The schedule for monitoring should therefore be determined by the treating physician and may be more frequent than the schedule of injections. If visual and anatomic outcomes indicate that the patient is not benefiting from continued treatment, treatment should be discontinued. For myopic CNV, a single injection is to be administered. Additional doses may be administered if visual and/or anatomic outcomes indicate that the disease persists. Recurrences should be treated as a new manifestation of the disease. The schedule for monitoring should be determined by the treating physician. The interval between 2 doses should not be shorter than 1 month.
Contraindications:
Hypersensitivity to aflibercept or to any of the excipients. Active or suspected ocular or periocular infection. Active severe intraocular inflammation.
Warnings and Precautions:
Intravitreal injections have been associated with endophthalmitis, intraocular inflammation, rhegmatogenous retinal detachment, retinal tear and iatrogenic traumatic cataract. Aseptic injection technique is essential. Additionally, patients should be monitored during the week following the injection to permit early treatment if an infection occurs. Patients must report any symptoms of endophthalmitis or any of the above-mentioned events without delay. Increases in intraocular pressure (IOP) were seen within 60 min. of intravitreal injection. Special precaution is needed in poorly controlled glaucoma (no injection while IOP is ≥ 30 mmHg). In all cases, IOP and perfusion of optic nerve head must be monitored and managed appropriately. Potential for immunogenicity. Instruct patients to report any signs or symptoms of intraocular inflammation, e.g. pain, photophobia, or redness, which may be a clinical sign attributable to hypersensitivity. Systemic adverse events including non-ocular haemorrhages and arterial thromboembolic events have been reported following intravitreal injection of VEGF inhibitors. Safety and efficacy of concurrent use in both eyes have not been systematically studied. No data are available on the concomitant use of Eylea with other anti-VEGF medicinal products (systemic or ocular). Risk factors associated with development of retinal pigment epithelial tear after anti-VEGF therapy for wet AMD, include large and/or high pigment epithelial retinal detachment. When initiating therapy, use caution in patients with these risk factors for retinal pigment epithelial tears. Withhold treatment in patients with rhegmatogenous retinal detachment or stage 3 or 4 macular holes. Withhold dose and treatment should not be resumed in event of a retinal break until break is adequately repaired. Withhold dose and do not resume treatment earlier than next scheduled treatment in event of: decrease in best-corrected visual acuity of ≥ 30 letters compared with last assessment; subretinal haemorrhage involving centre of fovea, or, if size of haemorrhage is ≥50%, of total lesion area. Withhold dose within previous or next 28 days in event of performed or planned intraocular surgery. Eylea should not be used in pregnancy unless the potential benefit outweighs the potential risk to the foetus. Women of childbearing potential have to use effective contraception during treatment and for at least 3 months after the last intravitreal injection of aflibercept. Populations with limited data: There is limited experience with treatment of patients with ischaemic CRVO and BRVO. In patients presenting with clinical signs of irreversible ischaemic visual function loss, the treatment is not recommended. There is limited experience in DME due to type I diabetes or in diabetic patients with an HbA1c over 12% or with proliferative diabetic retinopathy. Eylea has not been studied in patients with active systemic infections, concurrent eye conditions such as retinal detachment or macular hole, or in diabetic patients with uncontrolled hypertension. This lack of information should be considered when treating such patients. In myopic CNV there is no experience with Eylea in the treatment of non-Asian patients, patients who have previously undergone treatment for myopic CNV, and patients with extrafoveal lesions.
Undesirable effects:
Very common: Visual acuity reduced, conjunctival haemorrhage, eye pain. Common: Retinal pigment epithelial tear (known to be associated with wet AMD; observed in wet AMD studies only), detachment of the retinal pigment epithelium, retinal degeneration, vitreous haemorrhage, cataract, cataract cortical, cataract nuclear, cataract subcapsular, corneal erosion, corneal abrasion, intraocular pressure increased, vision blurred, vitreous floaters, vitreous detachment, injection-site pain, foreign body sensation in eyes, lacrimation increased, eyelid oedema, injection-site haemorrhage, punctate keratitis, conjunctival hyperaemia, ocular hyperaemia. Uncommon: Hypersensitivity (during the post-marketing period, reports of hypersensitivity included rash, pruritus, urticaria, and isolated cases of severe anaphylactic/anaphylactoid reactions), culture positive and culture negative endophthalmitis, retinal detachment, retinal tear, iritis, uveitis, iridocyclitis, lenticular opacities, corneal epithelium defect, injection-site irritation, abnormal sensation in eye, eyelid irritation, anterior chamber flare, corneal oedema. Rare: Blindness, cataract traumatic, vitritis, hypopyon. Description of selected adverse reactions: In the wet AMD phase III studies, there was an increased incidence of conjunctival haemorrhage in patients receiving anti-thrombotic agents. Arterial thromboembolic events (ATEs) are adverse events potentially related to systemic VEGF inhibition. There is a theoretical risk of arterial thromboembolic events, including stroke and myocardial infarction, following intravitreal use of VEGF inhibitors. As with all therapeutic proteins, there is a potential for immunogenicity.
On prescription only. Marketing Authorisation Holder: Bayer AG, 51368 Leverkusen, Germany.
Date of revision of the underlying Prescribing Information: July 2018.