Adalimumab promising in treating JIA-associated uveitis, study finds
Results from the Study Assessing double-masKed Uveitis tREAtrement (SAKURA) program support the efficacy and safety of intravitreal sirolimus 440 mcg (Opsiria, Santen) for treating noninfectious uveitis of the posterior segment, said Pauline T. Merrill, MD.
Adalimumab can be an effective treatment in children with juvenile idiopathic arthritis (JIA)-associated uveitis.
JIA-associated uveitis “is one of the most challenging inflammatory conditions in the pediatric population,” reported Bahram Bodaghi, MD, PhD, as there is little evidence-based data on therapeutic options, and glaucoma and cataract are the predominant complications (due to steroid treatment).
“There is an inconstant efficacy of methotrexate,” said Dr. Bodaghi, professor of ophthalmology, University of Pierre and Marie Curie, Paris. “We had promising results with the adalimumab and the infliximab in a case series and in our open-label trials when the study was designed in 2009.”
An earlier study found a relationship between laser flare values and complications of uveitis, with more than half of the patients reporting some complication during the follow-up period.
“In a pediatric population, using the Standardization of Uveitis Nomenclature (SUN) criteria have not yet been validated,” Dr. Bodaghi said. This led to a multicenter, randomized, investigator-initiated, placebo-controlled phase III trial comparing adalimumab with placebo at 16 sites in France which enrolled 31 children.
Adjuvite study details
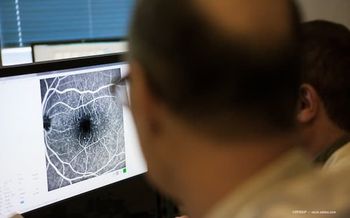
The primary endpoint was the efficacy of adalimumab versus placebo at 2 months, based on laser flare values.
There was flare reduction of 30% (evaluated by laser flare photometry [LFP]) compared with baseline and no worsening of flare and cells at slit-lamp, Dr. Bodaghi said. Further, efficacy was shown through tapering from months 2 through 12.
Researchers analyzed the transcriptomics on the blood of the enrolled children. Primary inclusion criteria included active uveitis associated with JIA, which could include polyarticular, LFP values > 30 photons perms for a normal below 7; resistance or intolerance to topical corticosteroids; resistance to systemic methotrexate used for at least 3 months; and possible evaluation of anterior chamber flare by LFP, and at least 4 years old weighing at least 15 kg (33 lbs).
Primary exclusion factors included any previous treatment with anti-tumor necrosis factor (TNF), contraindication to systemic immunosuppressants or biologics, and some ocular contraindications-such as chronic blood-ocular barrier rupture, impossible monitoring of flare by laser flare, uncontrolled glaucoma, or any major ocular complications.
The researchers considered responders those who showed a 30% reduction of flare values at month 2, with no worsening of inflammation based on the SUN criteria, Dr. Bodaghi said.
The study itself had two phases. During the initial 2 months, the patients were randomized to either placebo (n = 15) or adalimumab (n = 16), then all patients received adalimumab 40 mg every 2 weeks for 1 year. The second phase was an open-label phase.
Almost all the patients were female, (n = 15 in the adalimumab group, n = 13 in the placebo group), and both groups averaged about the same age (10 years), with each group having a duration of uveitis of about 4 years.
“The mean laser flare values were about 99 in the adalimumab group and 70 in the placebo group,” Dr. Bodaghi said. “The disease was bilateral in 63% of the adalimumab group and 93% in placebo group.”
There were 7 patients on oral steroids in the adalimumab group and 3 patients in the placebo group on oral steroids.
Intent-to-treat analysis
The intent-to-treat analysis showed significant results in the adalimumab group compared with placebo group, with 9 out of 16 responders at 2 months compared with 3 out of 15 in the placebo group.
“When there was a failure, the baseline flare values were very low, < 30 photons per ms,” Dr. Bodaghi said.
Although there were 6 serious adverse events in 5 patients, none were related to the study treatment.
“Overall, we found adalimumab was effective and safe in reducing ocular inflammation within 2 months and well tolerated over 12 months in patients with JIA-associated chronic uveitis and inadequate response to topic steroids and methotrexate,” Dr. Bodaghi said.
Results similar in UK
Results were similar to trial outcomes in the United Kingdom, “but separation was obtained earlier due to the use of LFP, which is a valuable tool to assess earlier improvement,” he added.
Dr. Bodaghi explained the group used the highest dosage possible before performing LFP to determine if the patient was still active.
“Below 30 photons per ms, it was very difficult to see the difference,” Dr. Bodaghi said. “We don’t know which patients might be methotrexate-resistant, as they were responding but did not have a complete response. In my opinion, every one of these children needed to go to biologics.”
Similarly, in some children with very active and severe ocular inflammation, the flare is “quite high” and even the use of aggressive corticosteroids will not decrease flare.
“It’s a chronic blood-ocular barrier that already has more damage than can be repaired,” Dr. Bodaghi said.
In France, methotrexate is still considered the primary first-line treatment, but the approval and use of adalimumab and anti-TNF agents alters the disease parameters, Dr. Bodaghi pointed out.
Patients are developing cataracts later in the course of the disease, but inflammation is better controlled. Time will tell if biologics will become embraced as readily as the first-line option.
Bahram Bodaghi, MD, PhD
E:
This article was adapted from a presentation Dr. Bodaghi delivered at the 2016 American Aacdemy of Ophthalmology meeting. Dr. Bodaghi is a consultant to AbbVie, Allergan, Bayer Healthcare, Novartis, Santen Pharmaceutical, and TxCell.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.