Chandelier-assisted technique shines for improving scleral buckling
By Cheryl Guttman Krader; Reviewed by John W. Kitchens, MD
Chandelier illumination for scleral buckling improves surgical control and precision during multiple steps of the retinal detachment repair procedure. That in turn translates into better outcomes for patients, according to John W. Kitchens, MD.
“With its benefits, chandelier illumination can rejuvenate enthusiasm for scleral buckling among retina specialists who are veterans of the procedure,” said Dr. Kitchens, private practice, Retina Associates of Kentucky, and voluntary faculty, Department of Ophthalmology, University of Kentucky, both in Lexington. “Because it provides a vitrectomy-like view, it may enable surgeons who were trained primarily in vitrectomy to convert to scleral buckling.”
Dr. Kitchens said he initially used chandelier illumination during scleral buckling in 2006 out of necessity because he wanted to record a teaching video of a novel external needle drainage technique.
“I realized during that experience that chandelier illumination could be useful in a variety of ways during scleral buckling,” he added.
The advantages
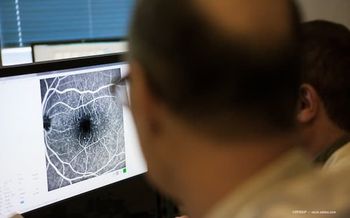
The advantages of the technique derive from obviation of the need for indirect ophthalmoscopy and its associated light issues and the ability to use a wide-angle viewing system through the operating microscope. Consequently, the chandelier-assisted technique enhances the identification of retinal breaks and their treatment with cryotherapy.
“With use of a wide-angle viewing system, the chandelier illumination-assisted technique gives better visualization of the peripheral retina, especially in cases where there is suboptimal media clarity, such as in eyes with corneal opacity or cataract,” Dr. Kitchens said.
But, the use of chandelier illumination is most appreciated while performing external needle drainage of subretinal fluid, he noted.
“In this technique, the surgeon penetrates through the sclera, choroid, and retinal pigment epithelium to reach the subretinal space using a 26-gauge needle attached to an open-ended syringe,” Dr. Kitchens explained. “It can be done with indirect ophthalmoscopy and a 20 D or 28 D lens, but obtaining good visualization with that approach is challenging because surgeons are simultaneously trying to control the view and the eye while also having to reconcile in the inverted image in their minds.”
Better visualization
Dr. Kitchens pointed out that working with chandelier illumination and looking through the microscope with a wide-angle viewing system gives better visualization with normal orientation of the image. Consequently, the surgeon is better able to judge the needle position, how close the retina is coming when it is reattaching, and the right time to extract the needle to avoid inadvertent retina penetration.
Chandelier illumination also enhances teaching because with its use, the mentoring surgeon shares the operating surgeon’s view and can see in great detail what the trainee is doing.
“There are some downsides of chandelier illumination, and those are the cost of the equipment itself and the disposables used for draping the microscope,” Dr. Kitchens said. “Those are minor tradeoffs, however, for the benefits of better precision and control.”
Advocating for scleral buckling
While the decline in scleral buckling and rise of vitrectomy for repair of rhegmatogenous retinal detachment is a controversial topic, Dr. Kitchens said that in his opinion, scleral buckling is underutilized and under-taught in vitreoretinal surgery training programs.
“The vast majority of eyes that I operate on for a failed repair performed by other surgeons had vitrectomy without a scleral buckle as their previous surgery,” Dr. Kitchens said. “Vitrectomy is faster than scleral buckling, it does not change the refraction in pseudophakes, and it may be favored for financial reasons, but our choice of technique should be guided by success. Compared with a primary scleral buckle or scleral buckle with vitrectomy, primary vitrectomy has a lower reattachment rate.”
Dr. Kitchens also noted that tracking success rates on a regular basis is an area where retina subspecialists can do better.
“Not tracking percentages of eyes that have successful repair of a retinal detachment is analogous to not keeping statistics for a baseball player,” he said. “Without tracking outcomes, it is impossible to know how well you are doing, and therefore, there is no foundation for making changes to improve.
“It is easy to calculate success rates for retinal detachment repair procedures,” Dr. Kitchens concluded. “It will help surgeons determine what they can do better and allow them to better serve their patients. Furthermore, surgeons ought to realize that even if they are not tracking their outcomes, in the future, private and government insurers will.”
John W. Kitchens, MD
This article was adapted from a presentation that Dr. Kitchens delivers at the 2017 Retina World Congress. Dr. Kitchens is a consultant for Alcon Laboratories.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.