Investigating surgical approaches for progressive retinal detachments secondary to retinoschisis
J. Fernando Arevalo, MD, PhD, investigated the anatomic and functional outcomes of pars plana vitrectomy, scleral buckle, or a combination of the two, and suggested that the combination approach may need further consideration.
Progressive symptomatic retinal detachment complicating degenerative retinoschisis (PSRSCR) is a rare complication of degenerative retinoschisis, but the treatment success rate following a single surgery is low compared with uncomplicated rhegmatogenous RDs.
J. Fernando Arevalo, MD, PhD, The Edmund F. and Virginia B. Ball Professor of Ophthalmology Chairman of Ophthalmology at Johns Hopkins Bayview Medical Center, Wilmer Eye Institute, Johns Hopkins University, Baltimore, investigated the anatomic and functional outcomes of pars plana vitrectomy (PPV), scleral buckle (SB), or a combination of the two, and suggested that the combination approach may need further consideration.
He explained that while progressive RDs that are secondary to degenerative retinoschisis can be asymptomatic in most patients, in the cases in which the RDs develop within the schisis, there is the potential for the RD to progress past the borders of the schisis and become symptomatic.
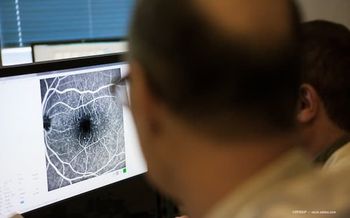
In the cases with limited progression, SB works well; but in more extensive cases (Figure) the optimal surgical approach is not yet established, he explained.
Determining the best treatment
Dr. Arevalo and his team [1] undertook a retrospective chart review of cases of PSRDCR from January 1, 2008, to December 31, 2019, and analyzed the patient demographics, surgeries performed, and the anatomic and functional outcomes associated with PPV, SB, or both. All patients underwent primary repair of PSRDCR, he described.
A total of 4,973 cases were identified during the study period and of those 36 eyes (0.7%) had retinoschisis with a RD. Ultimately, 18 phakic eyes of 17 patients (mean age, 54 years; range, 18-74 years) were included in the study and had a mean follow-up of 57 months.
Twelve eyes of 11 patients underwent the combination surgery, and 3 eyes of 3 patients each underwent PPV or SB. Six eyes, i.e., 3 in the combination group, 1 in the PPV group, and 2 in the SB group had another detachment.
Dr. Arevalo reported that all eyes had 1 or more outer layer breaks and 16 eyes (89%) had 1 or more identifiable inner layer breaks.
At the final evaluation, all eyes were attached for a final anatomic success rate of 100%. The overall single surgery anatomic success rate was 66%, i.e., 12 of 18 eyes were reattached. Eyes treated with PPV/SB had an single surgery success rate of 75%, PPV and SB had respective success rates of 66% and 33%.
The main culprit in the eyes that had another detachment was new retinal tears, he reported.
Complications following the surgical treatments included cataract in 78% of eyes at a mean of 11 months postoperatively.
Analysis of the functional outcomes showed that the mean best-corrected visual acuity (BCVA) for macula-on detachment was 20/20 at baseline and 20/25 at the final visit.The respective vision levels in the macula-off detachments were 20/50 and 20/100.
Considerations
PSRDCR occurs infrequently, with an incidence rate of 0.86/million individuals. Because of the low numbers of patients affected, Dr. Arevalo explained, no surgical treatment has emerged as superior for these patients.
The patients with macula-on RDs had better BCVAs both at baseline and the final evaluation.
Despite the high anatomic success rate, the single surgical success rate was 66%, which Dr. Arevalo pointed out, is significantly lower that the success rate associated with uncomplicated rhegmatogenous RDs. Thus far, no factors that are prognostic of the success rate have been identified. He suggested that the preoperative lens status and the role of vitreous base traction may be involved. “The addition of SB with PPV to reduce peripheral vitreous traction offers an alternative approach to lens removal,” Dr. Arevalo commented.
He concluded that while most of the current patients were treated with the combination surgery, the sample size was too small to facilitate a comparison with alternative surgeries and suggested that more research is needed to identify prognostic factors that are associated with poor visual and anatomic outcomes. The role of SB combined with PPV for PSRDCR requires further investigation.
Reference
1. Beatson B, Pham A, Ong SS, Ahmed I, Arevalo JF, Handa JT. Repair of progressive retinal detachment complicating degenerative retinoschisis: surgical management and outcomes in phakic eyes. Int J Retina Vitreous 2021;7:69.
Legend:
Figure: Wide-field color photograph of progressive symptomatic retinal detachment complicating degenerative retinoschisis. The white arrow to the right depicts the limit of the degenerative retinoschisis, the 2 white arrows to the left depict the limit of the progressive symptomatic retinal detachment (courtesy of Andres F. Lasave, MD).
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.