Noninfectious uveitis: Meeting the challenge
Chronic cases can be difficult for retina specialists; treatment is satisfying.
Noninfectious uveitis (NIU) is the third-leading cause of blindness in the United States. Its prevalence is estimated at about 121 cases per 100,000 adults and 29 per 100,000 children. Two out of 3 adult patients diagnosed with posterior segment NIU are of working age.1
NIU can range in severity and can be associated with systemic disease or injury; many cases are idiopathic. Posterior segment inflammation is associated with a higher level of vision loss, and about 1 in 3 patients will have systemic comorbidity.
There may be a perception that NIU cases, which sometimes necessitate ongoing involvement of specialists in other areas of medicine, are prohibitively time-consuming and difficult to coordinate; some retinal specialists may decline these patients altogether. But with the availability of FDA-approved and promising local and systemic therapies, the treatment of NIU can be a valuable and gratifying part of any retina specialist’s work.
First steps
Diagnosis begins with a comprehensive symptom review and a thorough exam of both the anterior and posterior segment. In my practice, we use a uveitis-specific questionnaire to assess relevant systemic symptoms. A systemic workup is initiated that includes laboratory testing for infectious and noninfectious etiologies, and a chest X-ray is also ordered.
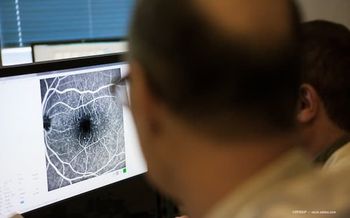
Once this foundation has been laid, ancillary testing including optical coherence tomography (OCT) and fluorescein angiography can provide valuable insight. Widefield angiography (fluorescein and/or indocyanine green) can be particularly helpful in patients with small pupils from synechiae, in whom detailed visualization of the posterior segment can be challenging.
OCT may be of value in diagnosing and monitoring a number of secondary complications of uveitis involving the macula; both cystoid and noncystoid macular edema, as well as vitreomacular interface disorders, can be markers of inflammation and are most objectively followed with OCT.
Likewise, OCT is useful for assessing the retinal pigment epithelium and the outer retina, aiding in both the diagnosis of NIU and delineating the precise location of the inflammation and cause of visual symptoms.
Fundus autofluorescence and infrared imaging can also be helpful, and for patients with media opacities that prohibit a view of the posterior segment, B-scan ultrasonography can be utilized.
Collaborating
Management of NIU, particularly when associated with systemic disease, can be time-consuming and can create unique challenges. This is in part because effective management of these cases often requires a collaborative, multidisciplinary approach to treatment, involving specialists in rheumatology, infectious disease, pulmonology, or oncology.
Such collaboration necessitates effective communication to coordinate patient care and a team approach for developing appropriate treatment plans. Some specialists may feel comfortable prescribing and managing steroid-sparing immunosuppressive therapy, but most choose to comanage with a rheumatologist or other specialist, as indicated.
Fortunately, there are a number of systemic therapeutic options for the management of NIU. It is imperative to involve the patient in the development of a treatment plan to ensure compliance and follow-up monitoring.
Often, for example, patients with NIU are of child-bearing age and may wish to avoid systemic therapies that would threaten fertility or have teratogenic potential.
Once patient concerns and needs are accounted for, many physicians suggest starting treatment with an antimetabolite such as mycophenolate mofetil or methotrexate or an anti-TNF agent such as infliximab (Remicade, Janssen Immunology) or adalimumab (Humira, AbbVie), which is FDA approved for this indication.2 Numerous other agents may be considered, alone or in combination, based on the specific condition, response to therapy, and comorbidities.
In many cases, ocular inflammation can also be controlled with the use of local steroids, delivered intra- or periocularly. Once again, there are a number of patient-specific factors to consider, such as systemic comorbidities, a history of ocular hypertension or known steroid response, laterality of the inflammation, and phakic status.
For some patients, local steroids may be the primary mode of therapy, and for others, local agents may be an adjunct to reduce the burden of systemic immunosuppression or for breakthrough inflammation.
Local treatment options
With its proven efficacy, safety, and ease of administration, the FDA-approved fluocinolone acetonide intravitreal implant 0.18 mg (Yutiq, EyePoint Pharmaceuticals) can be a game-changer both for some patients and the physicians who treat them. The sustained-release insert is delivered by an in-office intravitreal injection and delivers drug for up to 3 years.
In 2 randomized trials, patients receiving the fluocinolone insert experienced significantly lower rates of recurrent inflammation, which was the primary endpoint of the study. Improvement in macular edema, better visual outcomes, and less need for additional local therapy was also observed in both pivotal trials through 36 months. Adverse events included increased IOP and the development of cataracts. Need for glaucoma surgery was very low and comparable to control.3,4
Suprachoroidal triamcinolone (Xipere, Bausch Health) may soon be another effective treatment option. In recent trials of patients with NIU and macular edema, patients treated with the agent were 3 times more likely to gain 15 or more letters of vision, compared with the control group, which was the primary endpoint of the trial (47% versus 16% respectively, p < 0.001).
Treated patients also showed significantly greater reductions in central macular thickness compared with the control group (153 versus 18 μm, p < 0.001).5 This treatment appears to have a favorable adverse event profile and may be considered in certain patients, including those who are steroid responders.
In addition, the systemic immunosuppressant sirolimus is being evaluated (now in phase 3 studies) for intravitreal administration in NIU (intravitreal sirolimus 440 μg, Santen) and showing promise. If FDA approved, this treatment would be the first nonsteroid intraocular medication available for the treatment of NIU, potentially allowing patients to avoid steroid-related adverse events such as ocular hypertension and cataracts.6
Shifting mindset
Managing the care of patients with NIU within a retinal practice can be effective and rewarding but does require planning, coordination, and a willingness to work in tandem with other specialists.
It is essential that retina specialists have and maintain productive working relationships with skilled specialists who can assist in the management of NIU cases.
With diagnostic tools rapidly advancing and the current arsenal of both FDA-approved and off-label therapies available—as well as new treatments just around the corner—there has never been a better time for the retina specialist to consider managing NIU.
By taking on these cases and, when indicated, partnering with other specialists, retina specialists can preserve patients’ vision and forge loyalty that lasts many years.
In addition, working intimately with other subspecialties can be intellectually and personally gratifying. Patients with NIU represent an extraordinary opportunity to interact with the larger medical community.
REFERENCES
1. Thorne JE, Suhler E, Skup M, et al. Prevalence of noninfectious uveitis in the United States: a claims-based analysis. JAMA Ophthalmol. 2016;134(11):1237-1245. doi:10.1001/jamaophthalmol.2016.3229
2. Knickelbein JE, Kim M, Argon E, Nussenblatt RB, Sen NH. Comparative efficacy of steroid-sparing therapies for non-infectious uveitis. Expert Rev Ophthalmol. 2017;12(4):313- 319. doi:10.1080/17469899.2017.1319762
3. Jaffe GJ. Treatment of noninfectious uveitis that affects the posterior segment with a single intravitreal fluocinolone acetonide insert (FAi) – 3-year results. Presented: 2019 ARVO Annual Meeting; April 28-May 2, 2019; Vancouver, Canada.
4. EyePoint Pharmaceuticals announces positive topline 36-month follow-up data for second phase 3 study of YUTIQ. EyePoint Pharmaceuticals. Posted March 2, 2020. Accessed May 8, 2020.
5. Yeh S, Khurana RN, Shah M, et al. Efficacy and safety of suprachoroidal CLS-TA for macular edema secondary to noninfectious uveitis. Ophthalmology. 2019. doi:10.1016/j. ophtha.2020.01.006
6. Merrill PT, Clark WL, Banker AS, et al. Efficacy and safety of intravitreal sirolimus for non-infectious uveitis of the posterior segment: results from the SAKURA Program. Ophthalmology. 2020. doi:10.1016/j.ophtha.2020.03.033
POUYA DAYANI, MD
p: 213-483-8810
Dr Dayani practices at Retina-Vitreous Associates Medical Group in Los Angeles, California. He is a speaker for Regeneron, EyePoint, and Novartis, and has served on advisory boards for Allergan and Alimera.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.