NR600 retinal prosthesis: Safe with promising visual results
The first reported clinical results of a Phase I study following implantation of the 3-D neural interface retinal prosthesis showed it is safe in patients with end-stage retinitis pigmentosa.
Reviewed by Dr Peter Stalmans
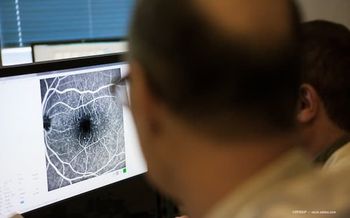
The first reported clinical results of a Phase I study following implantation of the NR600 Implant (Nano Retina Ltd.) indicated that this innovative three-dimensional neural interface retinal prosthesis is safe in patients with end-stage retinitis pigmentosa (RP), defined as no-to-minimal light perception.
The secondary endpoint, i.e., visual capabilities after the device was implanted, was also met, according to Dr Peter Stalmans, , a vitreoretinal surgeon from the Ophthalmology Department, University Hospitals Leuven, Belgium.
The NR600 is a stand-alone implant without wires that traverse the eye wall. Dr Stalmans explained that the device uses the natural eye optics and the retinal natural signal processing to provide the patient with vision. In this study, a miniature chip was implanted in the retina and held in place in the sulcus with haptics resembling those of an IOL.
The second component of the system is a set of wireless and rechargeable eyeglasses that provide the NR600 implant with power and communication through an infrared laser. The patient is able to fine-tune different stimulation structures and light settings with the push of a button.
The key principle of the prosthesis is the penetrating electrodes. Using this proprietary technology, a dense array of hundreds of three-dimensional microelectrodes penetrates the healthy retinal layers that originally received the signal from the photoreceptors.
The unique shape and structure of the electrodes enables precise, low threshold, local stimulation of the targeted healthy retinal cells, according to Dr Stalmans.
The prospective, multicentre, single-arm, interventional multinational study is being conducted in Belgium, Italy and Israel, with additional European sites planned. It began in the first quarter of 2020, with the goal of enrolling 20 patients with RP with minimal or no light perception.
The study design calls for an 18-month follow-up. The respective primary and secondary endpoints are safety and visual restoration, according to Dr Stalmans.
During the implantation procedure that included a standard lensectomy and vitrectomy, the NR600 Implant was inserted through a wide limbal incision and positioned over the macula.
Dr Stalmans reported that as of February 2020, three patients who are blind as a result of RP have undergone successful implantation of the implant at the Belgian site. The patients tolerated the procedure well and had no major signs of retinal or other ocular damage.
Six-month follow up clinical data is available for two of the patients. All patients could perceive visual stimuli upon activation of the implant.
At the first follow-up visual testing visit, conducted after the completion of the device parameter optimisation, all patients regained remarkable spatial vision, as well as orientation and mobility capabilities.
The patients experienced visual stimulus, and when subjected to the square localisation test were able to locate the square a number of times compared with baseline before the implantation, when it was practically impossible.
“It is impressive to see how patients that have lived for more than 5 years in complete darkness are able again to self-walk and can find and recognise objects around them,” Dr Stalmans stated.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.