Talking about genetics and AMD
Age-related macular degeneration (AMD) affects more than 10 million Americans, and the risk of developing AMD is increased when there is a family history. Yet, some people may carry the genetic variants without having a family history of the disease.
“Having regular eye exams can be incredibly helpful for detecting early signs of the condition and can give patients the opportunity to explore treatments and medications that can be used to slow the progression of AMD,” said Altovise Ewing, medical science liaison and genetic counselor,
But the issue on the advantages of genetic testing for AMD remains somewhat controversial.
While the American Academy of Ophthalmology’s task force on genetic testing said that “properly performed, interpreted, and acted on, genetic tests can improve the accuracy of diagnoses and prognoses, can improve the accuracy of genetic counseling, can reduce the risk of disease occurrence or recurrence in families at risk, and can facilitate the development and delivery of mechanism-specific care,”1, the group also recommended against “routine genetic testing for genetically complex disorders like AMD …”1
However, Awh et al. conducted a genetic analysis of patients enrolled in the National Eye Institute’s Age-Related Eye Disease Study (AREDS), concentrating on category 3 AMD in 1 eye and AREDS categories 1 through 4 AMD in the fellow eye from those patients enrolled in the AREDS who had available peripheral blood-derived DNA.2
The authors concluded people with moderate AMD “could benefit from pharmacogenomic selection of nutritional supplements.
In this analysis, patients with no CFH risk alleles and with 1 or 2 ARMS2 risk alleles derived maximum benefit from zinc-only supplementation. Patients with one or two CFH risk alleles and no ARMS2 risk alleles derived maximum benefit from antioxidant-only supplementation; treatment with zinc was associated with increased progression to advanced AMD.”2
Since those two papers were published, the Academy Task Force re-evaluated the issue, and found no reason to amend their earlier recommendations. The American Society of Retinal Specialists agreed with the AAO’s findings that genetic testing in AMD is not recommended.
But this is far from the end of the debate.
Two genes in particular (complement factor H and ARMS2/HTRA) have been closely associated with the disease. Complement factor H is a regulator of the complement pathway; unfortunately several studies failed to show any benefit of inhibiting the complement pathway in patients with AMD.3 The function of ARMS2/HTRA is not yet understood.
Macula Risk PGx is “a combined pharmacogenetic and prognostic DNA test to determine the patient’s risk of progression to advanced AMD based on their individual genetic risk profile and to aid in the selection of appropriate eye supplement formulations for a patient diagnosed with intermediate dry AMD,” according to the company.
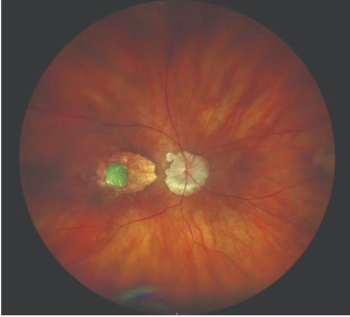
Macula Risk PGx combines a patient's current AMD status, genetic predisposition, and non-genetic risk factors to determine his or her 2, 5 and 10-year risk of developing advanced AMD, either geographic atrophy (GA) or choroidal neovascularization (CNV).
Macula Risk PGx has been validated in two large, independent populations where it was shown to have a 10-year predictive accuracy of 89.5%, with a sensitivity and specificity both > 80%.4,5
At this point, there is no definitive evidence that genetic information can help personalize treatment but future studies may change that. Patient perception of usefulness may also play a role.
A recently published study on public perceptions of hypothetical genetic testing results found significant associations between importance ratings and demographics variables, among others.6
In a survey administered at the 2015 Minnesota State Fair, 909 participants imagined that they had a blood test that looked at their genes and indicated that they were at high risk of developing one of three randomized conditions (Alzheimer's disease, macular degeneration, or colon cancer).
There were a total of eight categories:
1) medical management and communication;
(2) partner support;
(3) support and life fulfillment;
(4) diet and exercise;
(5) distal planning;
(6) religion/spiritual support;
(7) reproductive actions; and
(8) proximal planning.
Participants rated a wide range of actions as important, with medical management and communication and partner support receiving the highest mean ratings. Linear regression yielded significant associations between importance ratings and demographics variables (age and gender), genetic condition, and perceived severity of the condition for different action categories.
“Genetic counselors and other healthcare professionals should consider a variety of possible patient actions beyond medical actionability when discussing genetic testing results,” the authors noted.6
References:
1. Stone EM, Aldave AJ, Drack AV, et al. Recommendations for genetic testing of inherited eye diseases: report of the American Academy of Ophthalmology task force on genetic testing. Ophthalmology. 2012;119(11):2408-10.
2. Awh CC, Lane AM, Hawken S, Zanke B, Kim IK. CFH and ARMS2 genetic polymorphisms predict response to antioxidants and zinc in patients with age-related macular degeneration. Ophthalmology. 2013;120(11):2317-23.
3. Dunaief J. Should you receive genetic testing for age-related macular degeneration? Available at: https://www.brightfocus.org/macular/article/should-you-receive-genetic-testing-for-age-related-macular-degeneration-amd Accessed Feb. 1, 2019.
4. Seddon, J.M. et al, Validation of a Prediction Algorithm for Progression to Advanced Macular Degeneration Subtypes. JAMA Ophthalmol. 2013;131(4):448-455
5. Seddon, J.M. et al, The US twin study of age-related macular degeneration: relative roles of genetic and environmental influences. Arch Ophthalmol 2005; 23(3): 321-7.
6. Seiffert DJ, McCarthy VP, LeRoy B, Guan W, Zierhut H. Beyond medical actionability: Public perceptions of important actions in response to hypothetical genetic testing results. J Genet Couns. 2019. Epub ahead of print. doi: 10.1002/jgc4.1048
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.