When and how to treat myopic traction maculopathy
Myopic traction maculopa (MTM) and macular hole retinal detachments (MHRDs) are complex scenarios that demand accurate diagnoses and high surgical expertise. Internal limiting membrane (ILM) peeling and foveal-sparing ILM flap techniques are showing improved macular hole closure rates in difficult cases.
These pathologies fall into four categories, each of which requires a different treatment approach, according to Hiroko Terasaki, MD.
The first three categories-schisis only, schisis and retinal detachment, and full-thickness macular hole (FTMH)-are the prodromal stages of MHRDs, the fourth category, said Dr. Terasaki, who is chairman and professor, Department of Ophthalmology, Nagoya University, Graduate School of Medicine, Nagoya, Japan.
Simple schisis and schisis and retinal detachment
In eyes with schisis without a foveal detachment-i.e., schisis only-total ILM peeling is performed. At first, the posterior vitreous membrane and residual vitreous cortex are removed. Triamcinolone is injected again and the ILM is peeled gently.
"Correct diagnosis is the important factor," said Dr. Terasaki, describing an eye that had more than just simple schisis. Those eyes should be included in the group with foveal retinal detachments, which are seen clearly on swept-source optical coherence tomography (SS-OCT).
When considering these more complicated eyes, previous studies have reported that MHs develop in about 10% of eyes after total ILM peeling.
Interestingly, macular holes have been reported much less often or do not develop after ILM peeling that spared the fovea to treat myopic schisis, Dr. Terasaki noted.
Even in eyes with schisis only, schisis with a deep pseudohole, i.e., schisis shaped like a champagne flute, would be an indication for this method.
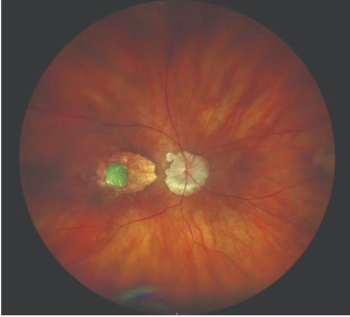
Case study
She described the case of a 76-year-old man with myopic schisis with a foveal detachments bilaterally who was treated with a foveal-sparing technique. In the right eye, the posterior hyaloid membrane, which resembles an ILM, was totally peeled. Triamcinolone was again injected and the ILM was peeled toward the edge of the fovea.
During the trimming procedure of this peeled ILM, Dr. Terasaki advised that the port of the cutter should always face in the direction opposite to the fovea.
In this case, Brilliant blue dye (BBD) was used to identify the ILM more clearly during trimming. An OCT scan performed intraoperatively showed the area of attachment of the trimmed ILM. In this case of one eye, the ILM was visible for at least 4 months postoperatively. She noted that an unpeeled ILM can become an epiretinal membrane (ERM).
In the second eye of this patient, after the posterior vitreous cortex was peeled, the ILM was stained with BBD. ILM forceps was used to peel the ILM toward the edge of the fovea. The flapping ILM was trimmed using the vitreous cutter, after which the ILM was peeled further up to immediately before the edge of the fovea to prevent postoperative ERM, Dr. Terasaki noted.
Use of OCT intraoperatively has an important function in cases such as these.
"Intraoperative OCT showed how close the ILM was peeled to the fovea," Dr. Terasaki said.
She demonstrated on spectral-domain OCT and SS-OCT images that the minute remnant of the ILM became invisible shortly after surgery in this eye.
Full-thickness macular hole
The third prodromal stage under discussion is that of eyes with FTMHs with and without schisis. In a study of highly myopic macular holes conducted at Nagoya University, two (6%) of 33 eyes failed to achieve closure of the macular holes after total peeling of the ILM. These holes were larger than 500 μm in the minimal diameter, Dr. Terasaki noted.
"The ILM flap technique has been recommended for large MHs," she said. "The macular hole closure rates have been generally good even in eyes with a long axial length."
She described the case of a 69-year-old woman with a high myopic MH with a minimal diameter of 627 μm. The inverted ILM flap technique to treat the MH was performed after the patient had undergone a previous failed vitrectomy. The ILM remained in the eye.
In the surgery under discussion, the ILM was peeled toward the edge of the MH, folded over, and slid into the edge of the MH using a diamond-dusted eraser. OCT images obtained intraoperatively showed the multi-layered ILM plugging the MH.
The technique used in this surgery was the classic multi-layered flap technique. However, other techniques exist, such as the single-layer technique, which is not performed for myopia. For large myopic MHs, gentle insertion is recommended.
Macular hole retinal detachments
The reported MH closure rates are low in these eyes following vitrectomy.
In light of this, Dr. Terasaki noted that the ILM flap technique has been recommended for all eyes with a MHRD. A 74-year-old woman with MHRD underwent vitrectomy and ILM peeling.
After the ILM was peeled to the edge of the MH and trimmed, the inverted ILM flap insertion technique was performed in which the ILM was inserted into the macular hole. Intraocular OCT showed that the ILM was in the macular hole.
Autologous neurosensory retinal free flap method has been reported recently to close a refractory MH in a 69-year-old woman who had undergone two previous retinal detachment surgeries in failed attempts to close the MH. During surgery, a retinal free flap was translocated from the periphery of the retina. The postoperative findings indicated that the macular hole was closed using the retinal flap from the periphery.
"Although this may work to prevent recurrence of the macular hole, the effect on the visual function has yet to be determined," Dr. Terasaki said.
Disclosures:
Hiroko Terasaki, MD
E:
This article was adapted from Dr. Terasaki's presentation during Retina Subspecialty Day at the 2017 meeting of the American Academy of Ophthalmology. Dr. Terasaki reported a financial interest in Carl Zeiss Meditec.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.