- Modern Retina Fall 2021
- Volume 1
- Issue 2
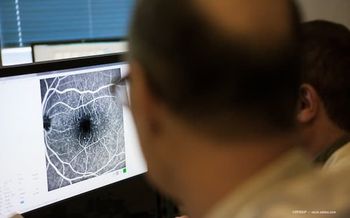
Addressing diabetic eye disease in senior patients
Confronting issues unique to aging may lead to better outcomes.
As cases of diabetes increase worldwide, the disease is accompanied by a precipitous increase in its most common complication, diabetic retinopathy (DR). At the same time, the aging population is growing, which is significant considering that the risk of developing DR increases the longer individuals live with diabetes and that the consequences of DR are unique in older patients.
In a recently published article, Ashay D. Bhatwadekar, PhD, and colleagues reviewed these issues to increase awareness and identify the best strategies for patient care.
“Understanding age-related retinal changes that increase vulnerability to DR in older individuals and age-related therapeutic challenges is essential for optimizing treatment of DR within the senior population,” said Bhatwadekar, an associate professor of ophthalmology at the Eugene and Marilyn Glick Eye Institute, Indiana University School of Medicine, in Indianapolis.
“Proper treatment of DR in [senior patients] could reduce the overall burden of diabetes.”
Age-related retinal changes
The authors pointed out that the retinal structure is altered with age in several ways. Macular blood flow decreases by 20% on average and the retina becomes thinner, with the change in thickness especially affecting the inner nuclear layer. In addition, the response of the microglia to injury slows, Müller cells become more susceptible to oxidative stress and the extent of lipofuscin accumulation in retinal pigment epithelial cells increases.
“The changes in blood flow that occur with aging may worsen ocular perfusion abnormalities in diabetes, and proliferation of microglia in the outer retina can contribute to proinflammatory responses,” Bhatwadekar said.
There are also age-related metabolic changes affecting the retina that are relevant for the development of DR. Disease-specific pathophysiologic mechanisms, such as accumulation of advanced glycation end products and the polyol pathway that contribute to oxidative stress, take advantage of the aging retina’s vulnerability that is associated with a defunct antioxidant defense system.
In addition, the effects of the VEGF pathway, which promotes angiogenesis, vascular permeability, and inflammation, could be augmented in the eyes of elderly individuals by the presence of a decreased retinal blood flow, Bhatwadekar explained.
Other DR pathogenic pathways that may be exacerbated by aging-related alterations relate to protein kinase C activation and hexosamine.
Clinical issues
Clinical studies of DR in aging individuals highlight the heightened concerns in senior patients. Not only does the prevalence of DR increase with age, but available evidence points to associations with depression and cognitive decline.
The article reviews current treatments for DR and diabetic macular edema, including a discussion of their mechanisms and role in clinical care. In addition, summary information is presented about emerging treatments that are being investigated in both preclinical and clinical trials. These include aldose reductase inhibitors that work by inhibiting the polyol pathway, a treatment that increases expression of sirtuin 1, protein kinase C inhibition and gene therapy to introduce VEGF genes. In addition, there is interest in sodium-glucose cotransporter 2 inhibition and angiopoietin-2 inhibition.
Treatment challenges
Highlighting the therapy-related challenges occurring in the senior population, the article discusses problems with medication adherence and age-related changes in drug pharmacokinetics and pharmacodynamics.
Anatomic and physiologic changes that occur with aging and the effects of medications that are commonly used by elderly individuals can lead to decreased absorption of orally administered drugs with the potential for reduced efficacy. Thus, the need may arise to consider modifications in the dosing regimen or delivery method.
As noted in the article, an increase in proteases within the vitreous that has been noted with aging suggests there may be age-related pharmacokinetic differences in drugs administered by intravitreal injection. Changes in drug distribution within the eye also may occur, and the potential for age-related differences in systemic distribution, drug metabolism and elimination also needs to be considered when investigating medications administered via an extraocular route.
Older individuals are more prone to medication nonadherence, which should be considered in their use of oral medications and in maintaining follow-up when receiving in-office treatments for diabetic eye disease.
“In the future, it is necessary to consider all of the above factors [when] treating senior patients with DR,” Bhatwadekar said. “Special programs directed toward tailoring and monitoring therapy may provide a better therapeutic outcome for [elderly patients].”
--
ASHAY D BHATWADEKAR, PHD
e: abhatwad@iupui.edu
Bhatwadekar is an ad hoc pharmacist at PCA Pharmacy. He reports no other relevant conflicts of interest.
--
REFERENCE
Leley SP, Ciulla TA, Bhatwadekar AD. Diabetic retinopathy in the aging population: A perspective of pathogenesis and treatment. Clin Interv Aging. 2021;16:1367-1378. doi:10.2147/CIA.S297494
Related Content:
Articles in this issue
about 4 years ago
Unraveling burdens of X-linked retinitis pigmentosaabout 4 years ago
Sustained drug delivery in ophthalmologyabout 4 years ago
Two new retinal surgical procedures for wet AMD: PDS and RGX-314over 4 years ago
Tackling teleretinal screening for diabetic retinopathyNewsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.