Researchers find Alzheimer disease detection potential in blood-based, retinal biomarkers
The recent study details the diagnostic value of a multimodal model utilizing both types of biomarkers when compared to unimodal models.
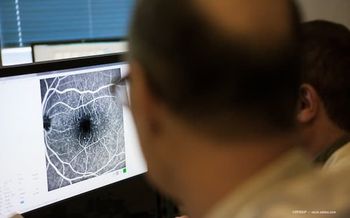
A recent study has further underscored the potential of retinal imaging as a noninvasive and accessible screening tool for Alzheimer disease in a multimodal model that utilizes retinal and blood-based biomarkers that have been used to detect the disease.1 The study, led by first author Swetha Ravichandran, PhD student at the University of Alabama at Birmingham, found that combining retinal and blood-based biomarkers significantly improved diagnostic accuracy, particularly when using threonine-217 (p-tau 217) and plasma amyloidogenic beta residue 42/40 ratio (Aβ42/Aβ40 ratio).1
“This could revolutionize early AD detection, facilitating earlier intervention, and improved disease management,” the study authors stated.
The study authors also noted that while previous studies have shown that blood-based and retinal biomarkers have shown potential to identifying patients that may be at risk for Alzheimer disease, integrating the 2 types of biomarkers have not been adequately assessed in preclinical Alzheimer disease.1 “This concept introduces a novel and synergistic approach to improve screening accuracy and predictive capability for early AD detection,” the researchers stated.
By using a multimodal receiver operating characteristic model based on retinal biomarkers (gliosis area, inner inferior retinal nerve fiber layer (RNFL) thickness) and plasma biomarkers (p-tau217 and Aβ42/Aβ40 ratio), researchers observed an area under the curve (AUC) of 0.97 (95% CI = 0.93–1.01) when compared to unimodal models of retinal and plasma biomarkers. Researchers also evaluated the diagnostic value of neurofilament light (NfL) and threonine-181 (p-tau181).1
“A single retinal biomarker may not be sensitive or specific to AD. This is because these retinal biomarkers are also affected by other retinal diseases. Even though we clinically excluded comorbid retinal conditions, it is difficult to distinguish preclinical manifestations of these comorbid retinal conditions from retinal changes that occur in preclinical AD,” the study authors stated. “For example, putative retinal gliosis is indicated in other retinal conditions that have neuroinflammatory components such as glaucoma, diabetic retinopathy, and [epiretinal membrane]. While the above retinal diseases were clinically excluded from our study, it is possible that some of the retinal changes observed could be preclinical manifestations of these conditions.”
A total of 82 cognitively unimpaired participants, and 141 eyes, who were previously involved in the Atlas of Retinal Imaging in Alzheimer’s Study (ARIAS) were included in the study. Inclusion criteria for the study included the absence of or controlled hypertension (blood pressure < 140/90), hyperlipidemia (total cholesterol ≤ 240 mg/dl), and systemic diabetes (HbA1c ≤ 7). All eyes in the study had a best corrected visual acuity of ≥ 20/40 (~ Log MAR 0.30) and refractive errors ≤ ± 3.00 DS (spherical equivalent) or equivalent axial lengths (range: 22–24 mm) in order to prevent any significant differences in the retinal magnification, per the Bennett formula.1
Participants also underwent comprehensive neuropsychological assessment using the MoCA and the RBANS-U. Spectral domain optical coherence tomography images were obtained, and plasma sampling and analysis was conducted for the study. With 32 participants having received recent Aβ PET neuroimaging, the results were also made available to the ARIAS study team.1
A significant correlation was also found between putative retinal gliosis and p-tau217 in the univariate mixed model (β = 0.48, p = 0.007) but not for the other plasma biomarkers evaluated (p > 0.05). Additionally, a sensitivity of 93.8% and a specificity of 92% was observed in the Aβ42/Aβ40 ratio.1
Study authors noted that future research should work to validate the findings of the study in larger, more diverse populations, in addition to evaluating the longitudinal impact of retinal changes in Alzheimer disease progression. Biological mechanisms linking the disease pathology to putative retinal gliosis could also provide an opportunity to understand more about said pathology and therapeutic targets.1
Reference:
Ravichandran S, Snyder PJ, Alber J. Association and multimodal model of retinal and blood-based biomarkers for detection of preclinical Alzheimer’s disease. Alz Res Therapy. 2025;17:19. https://doi.org/10.1186/s13195-024-01668-5
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.