Scleral buckle technique using PPV, laser photocoagulation
Scleral buckles and vitrectomy are the two main procedures used today to treat retinal detachments, with many surgeons performing a combination of the two.
By Margaret Wong, MD, Special to Ophthalmology Times
Scleral buckles and vitrectomy are the two main procedures used today to treat retinal detachments, with many surgeons performing a combination of the two.
Success rates for these two methods are comparable. Although studies show scleral buckling to be superior for phakic patients1,2 and vitrectomy superior for pseudophakes,2,3,4,5,6,7 I have seen a trend among new surgeons choosing vitrectomy over the gold standard of scleral buckles because the advancements in technology have made the procedure safer and easier to perform.
I tend to perform more vitrectomies when treating retinal detachments to avoid potential side effects of scleral buckles. However, when necessary, scleral buckles can be beneficial in closing retinal breaks, collapsing the space between the retina and underlying tissue, and re-establishing the anatomical connection between the two. My scleral buckle technique includes a pars plana vitrectomy and laser photocoagulation.
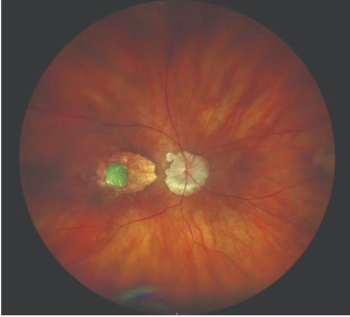
Series of fundus photographs of the scleral buckle effect in the periphery of the retina with laser scars overlying buckle and posterior to buckle. (Images courtesy of Margaret Wong, MD)
Scleral buckle technique
Patients who are good candidates for the scleral buckle technique are those who are phakic, have myopic retinal detachment, have retinal breaks that are clearly visible with the vitreous still attached, or have trauma cases with dialysis.
To perform the scleral buckle, I insert the speculum, and with scissors and forceps, make a 360º degree peritomy. I take down the conjunctiva 360º degrees around the cornea at the limbus to isolate the sclera.
I expose the sclera 360º degrees, move away the conjunctiva, and place a silicone scleral buckle around the eye. The band itself is 41 mm, while the sleeve that holds the band is 72 mm. I anchor the band with 5-0 mersilene sutures in all four quadrants on the sclera at the equator, then tighten it to the proper height.
Next, I make three incisions for the sclerotomy and proceed with the 25-gauge pars plana vitrectomy. Once the vitrectomy is complete and the vitreous is trimmed to a peripheral vitreous skirt, I check to ensure a posterior vitreous detachment is induced and the posterior hyaloid detaches.
A drainage retinotomy follows, using an extrusion device and perform an air/fluid exchange, draining the fluid under the retina through the drainage retinotomy. Once the retina is flattened, I switch to endolaser and begin treatment, lasering any tears present.
Good patient response
My patients respond well to this technique regardless of laser probe. However, when using a laser probe that is too large or bulky, it can be difficult to aim the beam into some areas of the eye.
For many years, I used laser probes from Alcon Laboratories and Iridex. Recently, I began using the Adjustable & Intuitive Extended Reach (A&I XR, IRIDEX) laser probes, and have found that they offer better control. In my experience, I have noticed increased efficiency and reduced complications.
These adjustable probes are extendable and, compared to standard laser probes, provide a farther reach by altering the probe from a straight configuration into a curved configuration. The far-reaching curve enables me to cover a greater range of angles, reaching areas that were difficult or impossible to treat without changing probes.
For instance, some areas posterior to the buckle indentation on the inside of the eye are difficult to reach with traditional laser probes. With the extended curve of the adjustable probe, I can deliver laser treatment, then turn the laser probe upside down and it will reach the area beneath the buckle.
In addition, the probe’s tighter cone lets me to adjust how close I am to the retina, which allows for increased ease of focus at a safer distance without sacrificing laser power. All of these features add up to more efficient and better anterior treatments.
Once endolaser is complete, I insert a gas bubble inside the eye, typically 14% C3F8, and then close the eye.
On occasion, if I cannot reach the retinal tears, I will utilize an indirect laser before closing. Prior to the adjustable probe, I would need to do this in about 80% of my cases. With the adjustable probe, this is rarely necessary.
Increased efficiency
Utilizing the new probe increases operating room efficiency and reduces complications. It extends to areas of the eye a surgeon is unable to reach with standard laser probes. I am able to remain seated during the procedure and I do not need to switch to an indirect laser.
There is less need for scleral depression. The staff has fewer steps to assist in the surgery, thus decreasing the number of errors that could occur. It also reduces overall surgical time.
It also is easier to view retinal tears and pathology when using the microscope with instruments inside the eye, versus the indirect ophthalmoscope. This contributes to a precise laser delivery. Precise laser treatments result in less surgery time and quicker recovery.
While scleral buckling has declined in recent years, it is a valuable and efficacious technique that should be utilized for the right patient. It is a treatment that takes skill and experience but is worth the effort.
References
1. Miki D, et al. Comparison of Scleral Buckling and Vitrectomy for Retinal Detachment Resulting from Flap Tears in Superior Quadrants. Jpn J Ophthalmol 2001;45(2), 187-91.
2. Mansouri A, et al. Recurrent Retinal Detachment: Does Initial Treatment Matter? Br J Ophthalmol 2010;94, 1344-7.
3. Stangos AN, et al. Pars-plana Vitrectomy Alone vs Vitrectomy with Scleral Buckling for Primary Rhegmatogenous Pseudophakic Retinal Detachment. Am J Ophthalmol 2004, 138:952-8.
4. Sharma YR, et al. Functional and Anatomic Outcome of Scleral Buckling Versus Primary Vitrectomy in Pseudophakic Retinal Detachment. Acta Ophthalmol Scand 2005;83, 293-7.
5. Brazitikos PD, et al. Primary Pars Plana Vitrectomy Versus Scleral Buckle Surgery for the Treatment of Pseudophakic Retinal Detachment: A Randomized Clinical Trial. Retina 2005;25, 957-64.
6. Weichel ED, et al. Pars Plana Vitrectomy Versus Combine Pars Plana Vitrectomy-Scleral Buckle for Primary Repair of Pseudophakic Retinal Detachment. Ophthalmology 2006;113, 2033-40.
7. Heimann H, et al. Scleral Buckling Versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment: A Prospective Randomized Multicenter Clinical Study. Ophthalmology 2007;114, 2142-54.
Margaret Wong, MD
P: 404-351-2220
Margaret Wong, MD is a board certified ophthalmologist with the Eye Consultants of Atlanta. She specializes in diseases and surgery of the retina, vitreous and macula, and inflammatory diseases of the eye, including uveitis.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.












































