Year brings advances in retinal imaging, screening, and gene/drug therapies
The topics of special interest to retina specialists during 2015 include optical coherence tomography angiography (OCTA) and screening for retinopathy of prematurity (ROP). Important research is taking place to determine the etiology of angiogenesis, possibly leading to targeting therapies in age-related macular degeneration (AMD), ROP, and diabetic retinopathy.
The topics of special interest to retina specialists during 2015 include optical coherence tomography angiography (OCTA) and screening for retinopathy of prematurity (ROP). Important research is taking place to determine the etiology of angiogenesis, possibly leading to targeting therapies in age-related macular degeneration (AMD), ROP, and diabetic retinopathy.
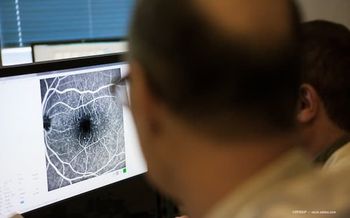
OCTA
Though the clinical utility of the technology is not yet well defined, research into this emerging technology is very active, according to Carl Regillo, MD, who explained that physicians are working to determine where OCTA ultimately will be most useful. Dr. Regillo is director of the Retina Service, Wills Eye Hospital, and professor of ophthalmology, Thomas Jefferson University, Philadelphia.
Such instruments commercially available to retina specialists include those from Carl Zeiss Meditec, Heidelberg Engineering, and OptoVue.
Julia Haller, MD, considered this technology to be amongst the most promising of the past year.
“One of the biggest advantages of the technology is that it provides a noninvasive way to image the retinal vasculature that provides a picture of the retinal layers,” said Dr. Haller, ophthalmologist-in-chief, Wills Eye Hospital, and professor and chairperson, Department of Ophthalmology,
Another possibility is that OCTA will enable the identification of early type 2 choroidal neovascularization (CNV) and treatment before the fibrous characteristics of CNV develop, but the natural history of these early lesions is also clear, according to Mary Elizabeth Hartnett, MD, professor of ophthalmology, John A. Moran Eye Center, Salt Lake City.
The first international conference on OCTA was held this August in Portland, OR.
David Huang, MD, PhD, and colleagues, as well as others worldwide, are testing OCTA with split-spectrum amplitude-decorrelation angiography (SSADA) and comparing it with standard imaging using fluorescein angiography (FA) and indocyanine green angiography (ICGA). Dr. Huang and associates have reported that SSADA-based OCTA seems better than FA and ICGA for managing ocular diseases. Investigators have conducted research into visualizing the vascular structures in wet and dry AMD, diabetes, arterial and vein occlusions, and glaucoma.
Screening for ROP
The prospect of streamlining the diagnostic process in ROP recently has been receiving more attention as a result of the findings of the 2014 Telemedicine Approaches to Evaluating Acute-phase Retinopathy of Prematurity (e-ROP) Study (Quinn et al. JAMA Ophthalmol. 2014 Jun 26. doi: 10.1001/jamaophthalmol.2014.1604).
The National Eye Institute study evaluated the “validity, reliability, feasibility and cost-effectiveness of a telemedicine system for detecting eyes of at-risk babies in need of a diagnostic examination by an ophthalmologist experienced in retinopathy of prematurity,” according to investigators.
Briefly, experienced ROP specialists trained readers who were not physicians in detecting ROP on digital retinal images. The ophthalmologist-director of the reading center supervised the readers. Based on the readers’ gradings, a computerized algorithm determined if referral-warranted ROP, which is plus disease, zone I ROP, and stage 3 or worse ROP, was present on the images.
The study found that screening can be useful for determining which patients have referral-warranted ROP.
The investigators reported: “These data suggest that the e-ROP system for training and certifying nonphysicians to grade ROP images under the supervision of a reading center director reliably detects potentially serious ROP with good intragrader and intergrader consistency and minimal temporal drift.”
“Instead of classifying a case as having severe ROP-that is, type 1 ROP-which is a diagnosis when treatment is considered, surgeons can look at individual cases with features that are reliable when evaluated on fundus images and that raise sufficient concern to consider a full examination and possible transfer to another institution for treatment,” Dr. Hartnett said. “This is especially helpful in rural areas of the United States or worldwide.”
In addition, physicians are actively evaluating the many challenges of telemedicine for detecting ROP.
Walter Fierson, MD, and Antonio Capone Jr., MD, published a detailed evaluation of the use of telemedicine systems for evaluating ROP (Pediatrics. 2015;135). Among the challenges they recognized when using such a screening system were the relatively few ophthalmologists who are qualified to be examiners in some areas and the remoteness of some neonatal intensive care units (NICUs).
However, the availability of wide-angle ocular digital fundus photography and the ability to transmit digital images to remote locations have led to the development of telemedicine-based remote digital fundus imaging evaluation techniques.
“These techniques have the potential to allow the diagnosis and monitoring of ROP to occur in lieu of the necessity for some repeated on-site examinations in NICUs,” they noted.
Home screening for visual changes
The Home Monitoring of the Eye (HOME) Study was an effort conducted by the investigators of the Age-Related Eye Disease Study 2 with the goal of determining if home monitoring by patients instructed in use of the ForeseeHome device (Notal Vision) could identify choroidal neovascularization while the patients still had higher levels of vision.
The results were compared with the standard of care, the Amsler grid. The HOME Study showed that at-home monitoring by patients may detect early disease progression and help preserve vision. This technology is a potential valuable spinoff of the AREDS2 study, according to Dr. Haller.
“More and more information currently is emerging about the value of early detection in AMD,” she said.
In July 2015, Allen Ho, MD, described the benefits of the device (Retina Today. 2015;66-68) as having a substantially lower rate of false positives than the Amsler grid and a sensitivity rate of 80%.
“The device accurately detects visual defects and distortions by measuring 500 retinal data points over 14° of a patient’s central visual field,” he said. “Each data point is measured three to five times in about 3 minutes.”
In addition, the noninvasive test can be performed quickly, after which the data are sent automatically to a data-monitoring center, where they are reviewed and sent to the patient’s physician within 2 to 3 days. The physician can then take the appropriate action if a substantial change in the patient’s test result is detected.
The data on the device “are compelling and speak to the medical adage that the sooner a problem is detected, the better the outcome with treatment will be,” Dr. Ho emphasized.
Research initiatives
Dr. Hartnett and colleagues are engaged in basic research that may translate into possible future therapies for sight-stealing retinal diseases. She is the Principal Investigator of a laboratory at the John A. Moran Eye Center that receives National Institutes of Health funding to study the mechanisms of normal and aberrant angiogenesis, particularly related to diabetic retinopathy, ROP, and AMD.
Despite the advances in treating retinal disease with anti-VEGF drugs, better and more targeted therapies are needed, Dr. Hartnett believes. To achieve this, she and her colleagues are looking at the downstream pathways from VEGF receptor signals or the co-receptors or proteins that interact with the VEGF receptors and cause overactivation of signaling pathways.
The investigators found that this overactivation of the VEGF receptor 2 signals contributes to both intravitreal angiogenesis and retinal avascularity by causing disordered angiogenesis of the endothelial cells, resulting in their growth into the vitreous instead of remaining in the retina.
In this study, Dr. Hartnett used a rat model of oxygen-induced retinopathy developed by John Penn, which represents peripheral severe ROP, to test aberrant blood vessel growth. They used a lentivirus to deliver a short hairpin RNA to VEGF-A or VEGF164 to only affect VEGF production in Müller cells.
“When we knocked down but did not knock out VEGF-A, we restored the normal growth of the blood vessels,” she said.
“Instead of the vessels growing erratically into the vitreous, they grew further out into the retina,” Dr. Hartnett said. “This study suggested that with the correct level of inhibition of the signaling pathways, the intravitreal neovascularization, which is stage 3 ROP, can be reduced and actually facilitate the normal development of angiogenesis.”
However, even with such a cell-specific approach to inhibit VEGF-A, changes in the retina occurred, but the status of the retinal function was unknown and these studies are ongoing.
The data from these experimental studies agreed with findings from clinical studies using anti-VEGF agents in infants with severe ROP, in which both inhibition of intravitreal neovascularization and facilitation of intraretinal neovascularization are seen.
But, there are safety concerns with even a single intravitreal injection of an anti-VEGF agent in a preterm infant, since VEGF is important in development and serum VEGF levels can be drastically reduced for up to 2 months, and in some infants, there is persistent avascular retina and late reactivation of intravitreal neovascularization.
Experimentally, when an intravitreal antibody was used in the rat model, the capillary density in the inner and deeper vascular network decreased.
“This finding provided some evidence for why there is reactivation of the neovascularization, such as occurs when anti-VEGF drugs are given to babies,” Dr. Hartnett explained.
Another possibility is that inhibiting VEGF reduces capillary density and stimulates other angiogenic pathways that are activated by hypoxia.
Additional anti-VEGF therapy may not affect intravitreal neovascularization induced by other angiogenic factors. Some investigators are treating persistent avascular retina with laser.
Erythropoietin is currently being studied in preterm infants for its neuroprotective effects, but there has been concern that it may be associated with angiogenetic effects depending on the time of administration, thus worsening ROP.
“We found that a mechanism appears to be through the erythropoietin receptor, which interacts with VEGFR2,” she said.
The laboratory is currently exploring funding options for this research.
Because Dr. Hartnett is focused on containing angiogenesis in the appropriate ocular compartments rather than inhibiting it, the laboratory is looking at mechanisms to reduce choroidal endothelial cell migration across the retinal pigment epithelium, which precedes most forms of sensory retinal choroidal neovascularization.
“We are looking at ways to inhibit the activation of choroidal endothelial cells to migrate,” she said. “One way appears to involve the interference with the generation of reactive oxygen species.”
The laboratory is also pursuing funding for this work through the National Eye Institute.
“We are conducting these investigations to determine disease mechanisms in order to find cures for blinding eye diseases,” Dr. Hartnett said. “However, importantly, we do not have the goal of inhibiting angiogenesis, but rather redirecting it to the areas that are hypoxic. It is counterintuitive to remove oxygen support and nutrients for tissues that need them.”
Julia A. Haller, MD
Mary Elizabeth Hartnett, MD
Carl Regillo, MD
Drs. Haller, Hartnett, and Regillo have no financial interest in any products mentioned in this report.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.