- Modern Retina Spring 2023
- Volume 3
- Issue 1
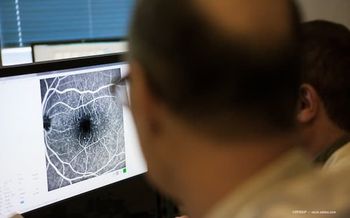
Suprachoroidal TA for macular edema caused by noninfectious uveitis
Reviewed by Steven Yeh, MD, FASRS
Combined data from phase 3 clinical trials showed the efficacy, safety, and tolerability of suprachoroidal space (SCS) triamcinolone acetonide (TA) for treating patients with macular edema caused by noninfectious uveitis. This result followed the favorable pharmacokinetics of suprachoroidal drug delivery demonstrated in preclinical data that indicated the potential for targeting diseased tissue, according to Steven Yeh, MD, FASRS, who reported his published findings1 at the Angiogenesis, Exudative, and Degeneration 2023 meeting.
Yeh is the Stanley Truhlsen Jr. Endowed Chair in Ophthalmology and director of retina and uveitis service at Stanley M. Truhlsen Eye Institute at the University of Nebraska Medical Center in Omaha.
Suprachoroidal injections
Triamcinolone acetonide injectable suspension (Xipere) received FDA approval to treat patients with macular edema secondary to uveitis in October 2021. SCS-TA is delivered between the sclera and choroid using the SCS Microinjector (Clearside Biomedical), and the treatment is distributed circumferentially and posteriorly in the SCS, Yeh explained.
This route both facilitates targeted delivery to chorioretinal structures, as opposed to intravitreal injection, and reduces the exposure of the nontargeted regions of the eye to drugs. To date, more than 1200 suprachoroidal injections of SCS-TA have been administered in clinical trials in 3 retinal disorders: uveitis, diabetic macular edema, and retinal vascular occlusion.
PEACHTREE and AZALEA studies
The PEACHTREE study (NCT02595398) was a randomized controlled trial in which patients with macular edema caused by noninfectious uveitis received either 4 mg of SCS-TA or sham injection at baseline and week 12. The AZALEA study (NCT03097315) was an open-label trial that included patients with active/inactive noninfectious uveitis with or without macular edema; these patients also received 4 mg of SCS-TA at baseline and week 12.
To enroll in these 24-week, phase 3 studies of SCS-TA, patients were required to have a central subfield thickness (CST) of 300 µm or more and baseline best-corrected visual acuities (BCVAs) of between 5 and 70 letters read (Snellen visual acuity 20/800 to 20/40). Analysis of the combined data of 95 patients showed substantial BCVA improvements of 15 or more letters; the BCVA in the SCS-TA group was 9.6 letters at week 4 and 13.9 letters at week 24. Significant decreases in the CST below 300 µm were seen at all follow-up visits.
The CST showed a mean change of –158.4 µm at week 4, with a sustained reduction throughout the study (mean change, –163.9 µm at week 24 vs −19.3 µm in the control group; P < .001).
More than 70% of patients with baseline inflammation had resolved inflammation at week 24. Patients treated with SCS-TA also had significantly lower rescue rates compared with controls. Ocular adverse events included eye pain or discomfort (~10%) and elevated IOP (12.6%).
Pearls for SCS-TA delivery
Yeh recommended using local anesthesia, including 2% subconjunctival lidocaine, and strict aspect techniques, including 5% povidone iodine. He administers SCS-TA using the following technique: The microneedle is positioned perpendicular to the surface to maximize microneedle length, then the conjunctiva is dimpled to ensure spreading of the conjunctiva. Finally, the drug is slowly and steadily injected to reduce the sensation of pressure from the choroidal expansion.
Reference
1. Yeh S, Henry CR, Kapik B, Ciulla TA. Triamcinolone acetonide suprachoroidal injectable suspension for uveitic macular edema: Integrated analysis of two phase 3 studies. Ophthalmol Ther. 2023;12(1):577-591. doi:10.1007/s40123-022-00603-x
Articles in this issue
almost 3 years ago
Early detection and treatment of DR and DME are essentialalmost 3 years ago
Photoreceptor viability may be a more promising target than GA in AMDalmost 3 years ago
Developments in gene therapy for inherited optic neuropathiesalmost 3 years ago
Vitrectomy: Is higher speed always better?almost 3 years ago
IOL designed for AMD offers hope for patientsNewsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.