- Modern Retina Fall 2022
- Volume 2
- Issue 3
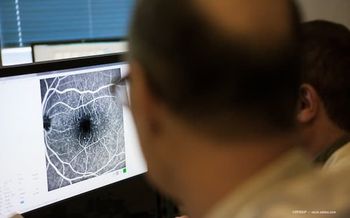
Acing the suprachoroidal injection for targeted drug delivery
This method of administration facilitates targeted delivery of the medication to the retina and choroid.
Reviewed by Steven Yeh, MD.
Xipere (triamcinolone acetonide injectable suspension; Bausch & Lomb) was launched recently as the first and only therapy approved by the FDA for use in the suprachoroidal space to treat macular edema associated with uveitis.
This method of administration facilitates targeted delivery of the medication to the retina and choroid.
“This injection procedure is a more nuanced technique compared with intravitreal injections and relies on delivering the medication to the suprachoroidal space, which is a low-resistance system,” said Steven Yeh, MD, professor of ophthalmology and director, retinal disease and uveitis, Stanley M. Truhlsen Eye Institute, University of Nebraska Medical Center, Omaha.
About 47% of patients with macular edema associated with noninfectious uveitis have a 3-line or greater improvement in visual acuity as a result of injection of triamcinolone acetonide, he reported.
Drug delivery pearls
Yeh emphasized the importance of discussing with patients that this injection technique is new.
Importantly, patient selection is paramount in that this technique of suprachoroidal injection is performed in patients with noninfectious uveitis with macular edema who likely will benefit from increased vision and reduced macular edema.
He prefers using subconjunctival lidocaine, although other physicians favor a topical anesthetic.
After applying the local anesthetic and antiseptic, such as betadine, he uses a 900 microneedle held perpendicular to the ocular surface to administer the drug to the suprachoroidal space. “This allows me to maximize the short length of the needle while delivering the drug reliably into the suprachoroidal space,” he explained.
The microneedle has a circular area that will create a small dimple in the conjunctiva, which allows the tissue to displace as the needle enters the suprachoroidal space. Yeh explained that as the plunger of the microneedle is depressed gently, he can feel the lessening of resistance as the medication enters the suprachoroidal space.
He also pointed out that the sclera has greater resistance and as a result this resistance can be felt if the needle is not positioned correctly within the suprachoroidal space.
“I deliver the medication with a very steady, slow, deliberate pace over about 5 seconds, in contrast to a rapid injection,” he explained, because patients may feel the expansion of the suprachoroidal space and pressure.
Bausch & Lomb has made a training platform available
The training accurately reproduces what the clinician should feel as the suspension is being administered, Yeh said.
Safety considerations
Injection of the drug into the suprachoroidal space can be associated with elevated intraocular pressure in about 12% to 14% of patients or development of cataract in about 6% to 7% of treated and sham-treated patients in the PEACHTREE study (NCT02595398).1
Development of endophthalmitis is also a possible adverse event, with an incidence rate of about 1 case in 2,000 patients who receive intravitreal injections.
Patient discomfort is possible when the drug is injected too rapidly or when the anesthesia is inadequate.
Physicians should also rule out the possibility of active infectious uveitis because of the potential for exacerbation of the disease with steroids.
“Xipere is an advance in drug delivery for the treatment of macular edema associated with noninfectious uveitis. I am excited about the possibility of where this drug delivery platform will go, both for patients with uveitis as well as other patients with retinal conditions for which this platform is currently being studies,” Yeh concluded.
Yeh is a consultant to Bausch & Lomb.
Reference
1. Yeh S, Khurana RN, Shah M, et al; PEACHTREE Study Investigators. Efficacy and safety of suprachoroidal CLS-TA for macular edema secondary to noninfectious uveitis: phase 3 randomized trial. Ophthalmology. 2020;127(7):948-55. doi:10.1016/j.ophtha.2020.01.006
Articles in this issue
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.