Wet AMD
Latest News


Lost to followup: Patients with AMD skip sight-saving treatment, experience vision loss
Latest Videos

CME Content
More News

The authors noted that the proportion of patients losing fewer than 15 letters from the baseline BCVA score in the study eye was comparable between the ranibizumab and biosimilar treatment groups.

The clinical trial is examining the efficacy of two doses of UBX1325 compared to every other month treatment with aflibercept through 24 weeks.

Roche’s treatment of faricimab is the first and only FDA-approved medicine targeting two distinct pathways, angiopoietin (Ang)-2 and vascular endothelial growth factor (VEGF)-A, that often cause retinal diseases that may cause visual loss.

Researchers found that the rate of visual decline increased significantly in patients with age-related macular degeneration during the COVID-19 lockdown who were followed over time.

LUNA trial will evaluate the 2x10^11 vg/eye (2E11) and a new lower 6x10^10 vg/eye (6E10) dose of Ixo-vec, with enhanced prophylactic steroid regimens in patients requiring frequent anti-VEGF injections. Interim data anticipated throughout 2023.

Regeneron announced that the primary endpoints were met in two pivotal trials investigating novel aflibercept 8 mg with 12- and 16-week dosing regimens in patients with diabetic macular edema and wet age-related macular degeneration.

The U.S. Food and Drug Administration has approved Coherus’ ranibizumab-eqrn (Cimerli) as an interchangeable biosimilar for all five indications of Lucentis.

Nancy Lurker, CEO of EyePoint Pharmaceuticals, shares the 12-month safety data from the DAVIO trial, investigating EYP-1901 for the treatment of wet age-related macular degeneration (AMD) and nonproliferative diabetic retinopathy.

According to EyePoint Pharmaceuticals, the clinical trial is reviewing EYP-1901, an investigational sustained delivery anti-vascular endothelial growth factor (anti-VEGF) treatment for wet age-related macular degeneration (wet AMD).

At ASRS 2022 in New York City, New York, Rishi Singh, MD, is presenting, “12-Month Results of EYP-1901 Vorolanib in a Bioerodible Durasert Insert for nAMD: The DAVIO Trial.” The Phase 1 trial showed a reduction in treatment burden over 12 months as well as a favorable safety profile.
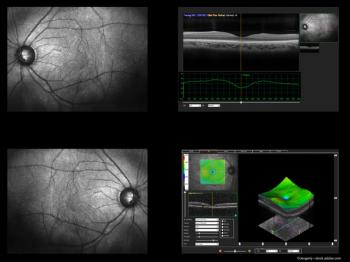
Investigators from Thailand took a close look at retinal fluid fluctuations in Thai patients with wet age-related macular degeneration (AMD) and devised a better way to measure the fluctuations in the central subfield thickness (CST).

Treatment with faricimab in patients with neovascular AMD achieved improvements in the visual acuity, central subfield thickness, and pigment epithelial detachments.
At ASRS in New York City, New York, Justis Ehlers, MD, presented a talk entitled, “Higher Order OCT Feature Assessments of the Impact of Fluid Dynamics on Visual Acuity in Neovascular AMD in a Phase III Clinical Trial: The Importance of Outer Retinal Integrity.” Here he discusses the findings.
A team of investigators from Johns Hopkins Medicine say they’ve discovered that levels of a specific protein appears to help accurately predict whether people with the wet form of age-related macular degeneration may need lifelong, frequent eye injections to preserve vision or if they can be safely weaned off the treatments.

Rahul Khurana, MD, offers updates and details about the Aaviate study, which is investigating a possibly once-and-done gene therapy option for macular degeneration via suprachoroidal drug delivery.

Justis P. Ehlers, MD, dissects the revelations from the data in the Phase 3 Hawk clinical trial regarding the impact of central subfield thickness, volatility and the overall impact on visual acuity.

Aleksandra Rachitskaya, MD, discussed the Phase 3 Archway end-of-trial results for the investigation of the Port Delivery System with ranibizumab in neovascular AMD.

Although off-label repackaged bevacizumab syringes appear to satisfy an urgent clinical and financial need for patients with a variety of retinal disorders, they are known to be associated with considerable public health concerns due to the risks posed to patients from compounding pharmacies’ lack of compliance with a variety of FDA requirements.

According to the study by a team of researchers from the University of California Irvine and University of Southern California, treatment with Humanin G reduced protein levels of inflammation markers that become elevated in age-related macular degeneration.

While the DAZZLE trial failed to meet its primary endpoint, KSI-301 demonstrated good initial visual gains and anatomic effects as well as positive durability.

The study will investigate the safety, tolerability, pharmacokinetics, and efficacy of AM712 in subjects with neovascular age-related macular degeneration.

Biogen and Samsung Bioepis announce the launch of ranibizumab-nuna and detail when the ophthalmic biosimilar will be available for retina specialists.

Outlook Therapeutics initially filed the BLA in March or the use of bevacizumab-vikg in the treatment of wet AMD. The company said it will re-submit a revised BLA by September.

The data presented at ARVO showed single subcutaneous doses of D-4517.2 were safe, well-tolerated in healthy subjects.

According to the ALOFT study, patients demonstrate improved long-term vision in real-world setting after wet AMD conversion compared to current standard of care.